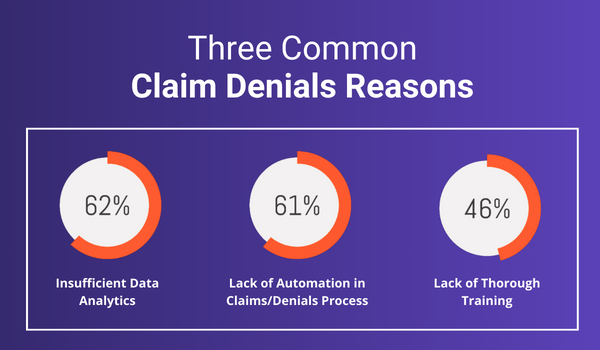
According to a previous survey, the top three reasons for an increase in claims denials are:
1. Insufficient data analytics
2. Lack of automation in the claims/denials process
3. Lack of thorough training
What many practices don’t realize is that with a few tweaks, they can drastically reduce claim rejections and truly optimize their revenue. Let’s walk through some steps your organization can take to minimize its number of rejected claims.
Automate Insurance Ineligibility
Insurance eligibility rejections occur when the patient is ineligible for coverage for a particular treatment under their current insurance. If this is the case, you’ll likely need to reach out to the patient to either get new insurance information or directly bill the patient. We suggest that practices always take the time to verify patient eligibility before rendering services and ultimately submitting a claim. Not only does this make life easier for billers, but it also improves the patient experience by ensuring they are not met with any unexpected charges.
However, the process of verifying coverage does not need to be as manual or cumbersome as calling the patient’s insurance provider. Cloud-based medical billing software that supports real-time eligibility verification can simply and effectively eliminate rejections that may occur due to a lack of eligibility. Real-time eligibility verification helps confirm patients’ insurance coverage and benefits with just a push of a button, ensuring confirmation before services are rendered, and greatly reducing downstream claim rejections. See how EZClaim does it.
Eliminate Mistakes With Automation, Claim Scrubbing, and Training
We are all human, and mistakes are bound to happen when doing manual data entry. These types of mistakes actually do cause quite a few claim rejections. Even the best medical biller will make mistakes from time to time, as a strong denial rate for a provider submitting claims sits at 5% or less.
Luckily, there are several steps providers can take to mitigate any coding mistakes or keying errors that can cause a claim to get rejected, and put your business in the best position possible to achieve this sought-after sub-5% rejection rate.
1. Claim Scrubbing: Checks claims for coding and keying errors and discrepancies before submission, allowing providers to address any issues proactively – reducing the risk of rejections.
Claim scrubbing may not tell you every possible reason your claim was denied, but it will catch simple coding and keying mistakes that are products of human error that your billers may miss.
2. Automation: Automating aspects of the claim submission process can greatly reduce the manual labor involved in the billing process while simultaneously improving accuracy by eliminating human error. The benefits of automation can be immense, as you can often process more claims, more accurately, in less time.
3. Staff Training: Lastly, be sure to spend the time and resources necessary to train your staff on how to properly use your billing software. A well-trained team that is familiar with its software’s capabilities is less likely to make mistakes, ensuring that claims are submitted accurately and have a higher chance of acceptance. Additionally, make sure your software vendor has strong support and onboarding teams that can upskill your team and provide any assistance when needed.
Eliminate Incorrect Patient Data by Integrating with your EHR
Whether it’s the misspelling of a name or the wrong ID number, incorrect patient data is a very common reason for claim rejections. Incorrect patient data is often a product of human error, and can be effectively eliminated by taking advantage of automation and integrations.
To avoid claim rejections for incorrect patient data, look to Integrate your cloud-based medical billing software with your electronic health records system. This integration enhances data accuracy, reduces duplicate entries, and streamlines the billing process, minimizing the risk of rejection. It also serves as an additional hedge against human error in the billing process by sharing key data and information that would otherwise have to be moved over manually.
Utilizing Reports to Become Proactive Rather than Reactive
If you’re experiencing repeated rejections for the same reason over and over – this could be a systemic issue. Some common systemic issues include:
- Claims not being filed on time
- Incorrect provider information
- Incorrect demographic information
- Wrong CPT codes
Cloud-based billing software with great reporting and dashboard capabilities is an absolute must to guarantee your practice can properly track its billing performance.
Create reports to monitor and analyze claim submission and acceptance rates. Your billing software should provide detailed reports that help you identify trends, address recurring issues, and continuously improve your billing processes. Here is a list of reports we recommend:
- Aging and Denial Reports
- Payment Posting Reports
- Adjustments Reports
- Provider Productivity Reports
- Patient Balance Reports
Minimizing claim rejections is a critical part of running a successful, efficient practice or billing company. Without robust cloud-based medical billing software in your corner, your practice may struggle to submit claims and realize revenue efficiently.
Are you ready to see what a cloud-based medical billing software can do for you?
Try EZClaim free for 30 days!