Apr 13, 2020 | Live Compliance, Medical Billing Software Blog, Partner
Since CMS HHS just updated their Telehealth regulations to adjust to the COVID-19 environment—including having a remote workforce—we wanted to provide a clear update to independent physicians and billers to advise them of the fast-moving changes of many regulations, and what to expect in the near future.
It is important to note that CMS has recently announced that new and established patients have availability to Telehealth, and HHS OIG is providing flexibility for healthcare providers to reduce or waive cost-sharing for Telehealth visits paid by federal healthcare programs. CMS is also expanding Telehealth services to people with medicare.
As a result, please see the below video from CMS which highlights the Medicare Coverage and Payment of Virtual Services and Telehealth.
In addition, we’ve included a few key questions and answers below. If you have further questions about Telehealth and your compliance, contact Jim Johnson with Live Compliance at Jim@LiveCompliance.com or (980) 999-1585.
1. Who can provide Telehealth services?
-
- Physicians
- Nurse Practitioners
- Physician assistants
- Nurse-midwives
- Certified nurse anesthetists
- Clinical psychologists
- Registered dietitians
- Nutrition professionals
2. What services can a medicare beneficiary receive through Telehealth?
-
- Evaluation and management visits (common office visits)
- Mental health counseling
- Preventive health screenings
- More than 80 additional services
3. What are the types of virtual services?
-
- Medicare Telehealth visits
- Virtual check-ins
- E-visits
- Telephone services
Live Compliance is an EZclaim premier partner for HIPAA compliance and is integrated into EZclaim’s billing solution.
If you have any further questions about Telehealth regulations and your compliance, e-mail Jim Johnson at Live Compliance at Jim@LiveCompliance.com, or phone him at (980) 999-1585.
[ Contribution by Jim Johnson with the Live Compliance ]

Apr 13, 2020 | Medical Billing Software Blog, Trizetto Partner Solutions
On January 13th we posted part one on this topic of Eligibility in healthcare, in that, we touched on deductibles, co-pay, and max out-of-pocket pay. Now in part two, we review the impact of price transparency in healthcare and its importance to the healthcare team decisions.
Consumers are the most important member of the healthcare team and are better collaborators in their care when they know all the variables and their required responsibilities in the process.
The individual consumer’s healthcare team includes, along with themselves, the physician and their staff, the pharmacist, an insurance adviser, and possibly some gatekeepers as well. The communication of clear symptoms when a patient is diagnosed is the responsibility of that team along with building an understanding of the financial responsibility that goes with any medical solution. While providing answers, options and solutions is a provider’s responsibility, so is providing a cost for the provided care. Therefore, price transparency can be achieved when the cost for that care is presented in a clear and concise fashion so the patient can understand what they owe, why they owe it, and when it is due.
Ensuring your staff is educated on discussing the financial responsibility with the patient from the first appointment and forward will strengthen the healthcare partnership and assist in the collection process. Understanding the steps that occur post the upfront estimate can be beneficial to the team. This discussion can be bolstered by ensuring bills are clearly marked with the statement, “this is a bill”, also clearly listing what the patient is being charged for when the bill is due and offering details on the methods of payment that are accepted. This clarifies what insurance will cover for the patient and their own out-of-pocket cost, prompting them to share any concerns and constraints with payments upfront.
Estimating patient responsibility is one part of the reimbursement process that is used for transparency for patient billing. The estimates can be provided using a spreadsheet of prior reimbursement and your most commonly billed CPT codes. If you would like an automated and more accurate option then look into a software tool like the Patient Responsibility Estimator by our solutions partner, TriZetto Provider Solutions (TPS). Giving this to the patient at the time of checking in will assure they have a rough idea of the costs and allow the office to collect upfront if needed.
For more information on how EZClaim can help you with this journey, schedule time with our sales team. Ready to get started? Download your FREE 30-day Trial today!
[ Contribution by Brenda Smelser with the DMC ]

Apr 13, 2020 | Medical Billing Software Blog, Revenue, Trizetto Partner Solutions
Because of COVID-19, some practices are doing triage from the car before they will allow a patient into their offices. Practices should also take a ‘cue’ from this by instituting protective measures for their finances.
I went to the doctor for a regular visit last week, which seemed anything but regular. I sat in the car and called to let them know I had arrived. They verified my demographics and insurance information over the phone; me in the parking lot, them in the office. The MA came out with her PPE and took my temperature, found me to be fever free so I could enter the building.
My nurse practitioner came in for our visit. We went about our appointment as usual except this time she took my superbill upfront herself and handed it to the check-out staff member. We scheduled a Telehealth visit instead of a traditional office visit. At the checkout desk, I said “I’m pretty sure I have a balance from the last visit, can I take care of that today?”. I loved where their heart is at, but I was sad to hear her say “You do, but we aren’t worried about that today. Just pay when you get the next statement.”
With so many things in chaos right now, so much thrown at you, and out of your control – let us not forget about the protective measures you can put in place for your practice. This is the time to get some vitals and triage from the car, before blindly allowing the chaos into your business. So, what should you be tracking?
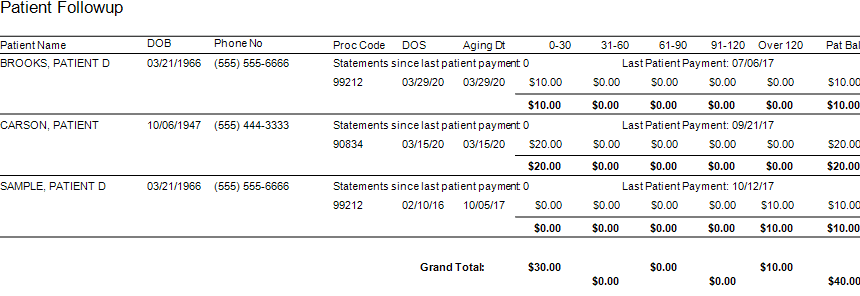
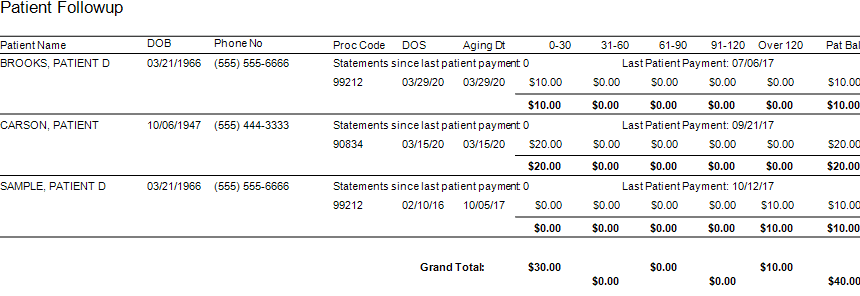
Start with basics – look at the aging balances. More than likely, you have money on the table! In EZClaim, you have the option to run full aging, but the more efficient option is running the Insurance Follow Up report and the Patient Follow Up report. Just running these reports will let you know where there is money that needs to be collected. In addition – it just may show you that it is time to reevaluate policies and procedures in your office related to patient balances and insurance follow-up. Here is a peek at what these two reports can do for you.
Patient Follow Up Report: This report will show you balances that are outstanding with your patients. While this may not be the easiest time to ask patients to pay their balances, there are steps you want to consider:
- Consider what you will do with lingering patient balances. The Patient Follow Up report will show how many statements have been sent since the last patient payment. If you have sent several statements is it worth continued efforts?
- Contact your patients to see if they can pay with an HSA or FSA account
- Offer to set up a payment plan
- Write off the balance as a bad debt or a one-time professional courtesy
- Consider sending the account to collections
- Use technology to your advantage. Take this time to consider enabling online payment options.
- Create or revise patient payment policies and train your staff on these policies
Insurance Follow Up Report: This report will show your balances that are outstanding with insurance companies. Some of the useful features of this report include:
- Ability to see the aged balances by the payer. This lets you get the biggest bang for your buck. Look for payers that have a large percentage of balances in the oldest buckets and work those first.
- All the information you need for calling the insurance is right there on the report. You will have easy access to the date of birth, member ID number, and claim totals on the report.
- During your research, you will find common themes. Use these themes to update your office procedures and train your staff to eliminate errors so that claims get paid quicker.
EZclaim billing software can help you manage your office’s finances. Visit our website to find out more about our solutions: https://ezclaim.com/
[ Contribution by Stephanie Cremeans with EZClaim ]
Apr 13, 2020 | Alpha II, Medical Billing Software Blog, Partner
One of our partners, Alpha II, is presenting a special webinar on COVID-19 billing changes on April 16, 2020, “COVID-19: Critical Coding and Regulatory Updates,” to provide the most up-to-date information on the coming changes to new procedures, diagnosis codes, telehealth updates, and changes to regulatory policies.
As guidelines for coding and billing of COVID-19 services are revised almost daily, rest assured Alpha II is working to implement these critical changes to regulations and coding guidance as quickly as possible by conducting near-daily promotions.
Here is a very brief summary of some of the updates we’ve implemented:
-
- Clarification of correct telehealth rendering POS and use of modifier -95
- Modification of diagnosis code edits for billing of COVID-19 symptoms from February 20 – March 31, 2020, and use of new diagnosis U07.1 for dates of service on or after April 1, 2020
- Addition of the new AMA CPT code 87635 effective March 13, 2020
- Addition of the new CMS CPT codes U0001 and U0002 retroactively effective February 4, 2020
- Modification for waiver of DME replacement requirements prior to March 1, 2020
- Modification for waiver of occurrence code 70 on SNF three-consecutive day stay validation prior to March 1, 2020
- Modification to LCD/NCD edits to relax rules related to respiratory-related devices and services
- Modification to Medicaid for the temporary suspension to prior authorization rules in PHE areas effective March 1, 2020
You can get all the latest COVID-19 specific updates here: https://www.alphaii.com/landing/covid19
Alpha II is an EZclaim partner that provides “Claim Scrubbing” for our medical billing software system. View our website for more details on this: https://ezclaim.com/partners/

Apr 13, 2020 | BillFlash, Partner
Medical billing managing collections during COVID-19 will be different than it was in the past. It has already changed a lot about how medical practices operate, and in a short amount of time. One thing that hasn’t changed, however, is that practices need to get paid in order to continue operating. This includes sending patients to collections when necessary.
Managing late or unpaid bills during economic uncertainty may require a different approach than you’re used to. Before you send patients to collections, make sure you take these steps first.
- Be upfront about payment expectations from the beginning
-
- You should already have a strategy in place regarding informing patients how much they owe for services. Stick to it. Many people are hoping for leeway on certain bills due to the economic impact of COVID-19, but gently remind your patients that for essential healthcare services to continue, practices need to keep revenue flowing, and that means billing will continue as usual.
- Set up payment plans
-
- If a patient is unable to pay a bill in full, help them set up a payment plan. BillFlash PlanPay lets you set up scheduled, automatic payments to be paid over a set period of time. This is the best option for both you and the patient because:
- The patient has a more manageable bill
- Your practice is more likely to be paid in full
- Setting up a payment plan shows your patients you’re willing to work with them. That’s usually all they need to be assured that you care.
- Send out multiple reminders
-
- Use whatever resources you have—email, phone, text, mail—to contact patients about balances they owe. Be courteous in your reminders, but firm. Most patients want to pay their medical bills. Often all they need is a simple reminder and an easy way to make the payment.
- BillFlash helps you manage all of this during the pre-collections phase to help ensure you are paid as quickly and completely as possible.
If none of these steps work, then it’s time to get collections involved.
What to Include in a Collections Letter
Include all the facts of the visit. This includes:
-
- Date of service
- Service provided
- Amount patient owes
- Payment options
Tone of the Letter
The right tone in your letter can do more to ensure payment and a continued relationship with the patient than anything else you include. You need to convey a sense of urgency, but without being overbearing and intimidating.
A few tips to keep in mind:
-
- Empathize with the patient. Simply saying “We understand you may be experiencing financial difficulties at this time” is more likely to get a response than a curt “final warning” threat.
- Explain why it is important for the patient to pay anyway. Example: Like any other business, our practice relies on revenue to thrive. In order to continue to provide these valuable healthcare services, patients need to pay their bills in full and on time.
- Offer a payment plan. Give patients one more opportunity to pay their bills in smaller chunks over a period of time to avoid having their accounts sent to collections.
We’re all experiencing difficulties during this global pandemic. The only way to get through it is to work together. Being upfront with patients about payment expectations and being willing to work with patients who have fallen on hard times will help all of us through this global health crisis.
BillFlash Collections Services can help you in managing collections during COVID-19, and simplify and streamline all your other collection processes for you, saving you the headache of exporting, importing, and working with a disconnected agency.
As an EZclaim ‘preferred’ partner, BillFlash is fully integrated with the EZclaim Premier billing application. For more details, view this informational video: https://www.rcm.billflash.com/ezclaim For more information about the EZclaim billing solution, view our website: https://ezclaim.com/