May 14, 2022 | EZClaim
Reporting is a fundamental tool in EZClaim and key to medical billing success. With EZClaim’s powerful reporting capabilities, your business decisions can be informed by real-time data and not left to chance. From adjustment reports to patient demographics, EZClaim comes with a range of baseline reports that every biller needs to work cleanly and efficiently.
Why these reports are critical for your business
Accurate and timely reporting is crucial to maintain a full awareness of your business and address issues before they become critical. With the right reporting tool in place, you can avoid lost revenue, keep reimbursements high, and decrease denials.
EZClaim provides insight to key revenue cycle metrics and makes it easy to identify month to month trends. Whether it is a payments report that shows a sudden drop in collections or an aging report for claims that have not been paid in a month or longer, these reports allow you to identify problems and take action before it is too late.
The features that set EZClaim reporting apart
On demand reporting formatted your way
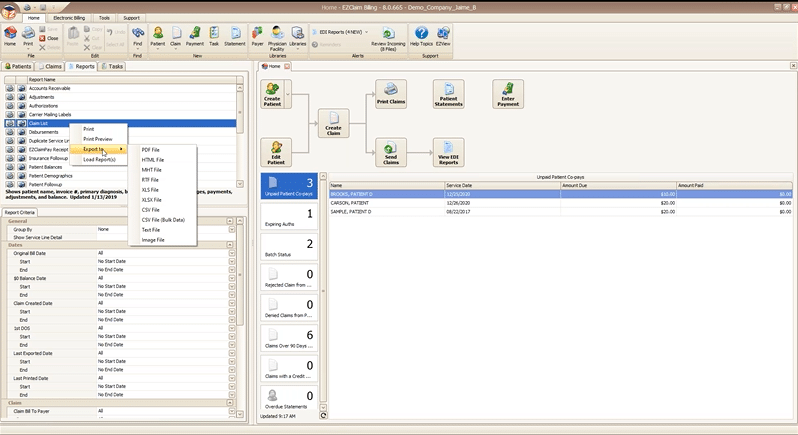
All EZClaim reports can be exported in a variety of formats so that you can open them directly in the format you most prefer. In two clicks you can preview and print a hard copy of any report, or export and open on your desktop.
Reports can be exported as a:
- PDF file
- HTML file
- MHT file
- RTF file
- CSV/XLS/XLXS (Excel) file
- Text file
- Image file
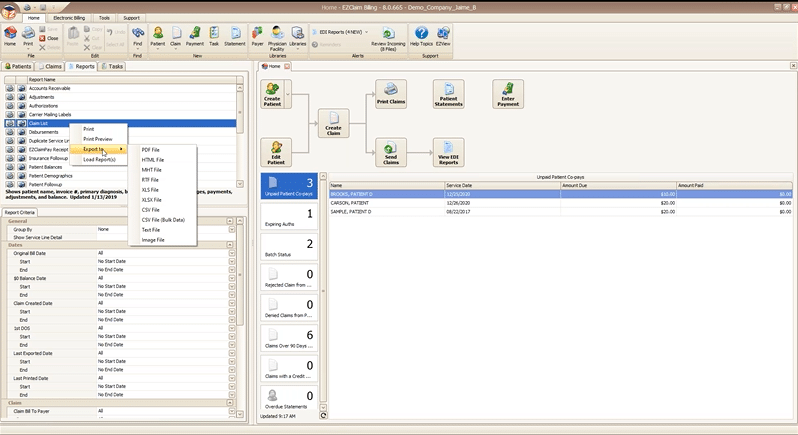
Getting just the data you want with report criteria
Every report in EZClaim can be tailored to show only the data you want by specifying report criteria. Report criteria parameters vary by report but aim to give you full control over what the report returns. For example, the “Claim List” report provides a list of claims and their associated details, such as invoice number, payments, adjustments, and more. This report provides a wide range of criteria options so that you can return only claims that, for example, fall in a particular bill date range, or claims for a specific payer. The best part is that you can combine as many criteria parameters as you need to zoom in on just data that you want.
With these features, EZClaim makes reporting powerful and flexible, by giving you the power to instantly create real time reports that are as focused or broad as needed, and then exported in the exact format that you need them.
If you are ready to learn more about EZClaim reporting or have any questions about our leading medical billing software, schedule a consultation today or get in touch with our experts.

May 12, 2022 | Health eFilings, Partner
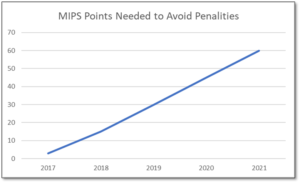
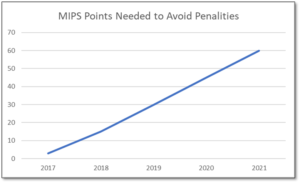
MIPS is a point-based program and understanding how to earn MIPS points is critical to avoid a 9% penalty. The MIPS program continues to change and evolve each year as it meets the goals laid out in the MACRA law and carried out by CMS. Since the program was implemented in 2017 the points threshold to avoid a penalty has grown from 3 to 60 out of a possible 100 MIPS points; the penalty has increased from 3% to 9% of annual Medicare reimbursements; and, the number of patients required to be reported on has increased from 20 patients to all patients for all payors. With the rules changing every year, the strategy you previously used to score MIPS points and report may no longer be optimal. If you want to avoid the 9% penalty in 2021 and beyond, you must think differently and evolve your strategy for MIPS.
With all the complexities and nuances of the program, it’s challenging to know what you can do to impact your MIPS score. Here are three critical considerations that provide guidance on ensuring you have the right MIPS strategy to optimize your ability to earn MIPS points for the 2021 reporting period.
The Quality Category, worth the most points, is the category to focus most of your effort. Because the Quality category is worth anywhere from 40 to 85 MIPS points, focusing on this category throughout the year is critical. You need to submit a full year’s worth of data so now is the time to ensure that you are capturing all relevant data in your EHR and or billing system so that it can be properly extracted and reported on for your submission.
40% of the MIPS points require you meet stringent timeframe requirements. Two of the MIPS categories, Promoting Interoperability and Improvement Activities, have timeframe requirements where you must perform and document activities for a minimum of 90 continuous days. These are not easy categories in which to be successful and so if you wait too long you will find it impossible to put the right actions in place to complete the activities necessary to earn any of the MIPS points in these categories.
The reporting methodology you choose impacts the points you can earn. Not all reporting methodologies are the same and the reporting methodology you select has a significant impact on the MIPS points you could earn. Unless you select a reporting partner that will help you earn the most points available by leveraging technology to facilitate the ease, accuracy, and completeness of tracking and reporting to maximize your score, you risk leaving MIPS points on the table and significantly sub-optimizing your score. Reporting via a CEHRT, like Health eFilings, is the best approach because it optimizes the MIPS points that could be earned and therefore, maximizes Medicare reimbursements.
Health eFilings’, a CEHRT, is the national leader in automated MIPS reporting and our cloud-based ONC certified software fully automates the MIPS reporting process. And because Health eFilings’ service is an end-to-end electronic solution that doesn’t require any IT resources, administrative support, or workflow changes, you will save significant time while maximizing your financial upside.
Contact Sarah Reiter, sreiter@healthefilings.com, or 608.841.1866 to find out how to maximize your reimbursements and protect your bottom line.
About Health eFilings:
Health eFilings, a CEHRT, is the national leader in automated MIPS compliance and quality data analytics. Its services drive improved patient outcomes, optimized quality measures, and stronger financial results for healthcare practices. Their proprietary cloud-based ONC certified software is significantly more efficient and effective than any registry as it does all the work to extract, calculate, benchmark, format, and electronically submit MIPS data to CMS so clients avoid significant penalties and earn maximum reimbursements. And, you can have peace of mind knowing you are working with the best partner because CMS has accepted 100% of Health eFilings’ submissions. Learn more here: https://healthefilings.com/ezclaim
ABOUT EZCLAIM:
EZClaim is a leading medical billing and scheduling software provider that combines a best-in-class product, with correspondingly exceptional service and support. For more inforatmion, schedule a consultation today, email our experts, or call at 877.650.0904.

May 5, 2022 | HIPAA, Live Compliance, Medical Billing Software Blog, Support and Training
Your organization’s annual HIPAA Security Risk Assessment and Analysis are only one element of the compliance process, and whether you’re a Business Associate or Covered Entity, your organization must also “implement security updates as necessary and correct identified security deficiencies”. In other words, you must act via a Corrective Action Plan (CAP) following the required risk assessment process.
Here are a few common Corrective Action Plan steps:
- Implement technical policies and procedures to allow access only to those persons or software programs that have been granted access rights to information systems maintained.
- Implement procedures to regularly review records of information system activity, such as audit logs, access reports, and security incident tracking reports.
- Conduct accurate and thorough assessments of the potential risks and vulnerabilities to the confidentiality, integrity, and availability of ePHI.
- Develop a complete inventory of all its categories of electronic equipment, data systems, and applications that contain or store ePHI, which will then be incorporated into its Risk Analysis, and must complete a Risk Management plan.
What happens if I fail to complete my Security Risk Assessment?
Failing to complete your annual Risk Assessment oftentimes means the organization will be required to complete a “robust” Corrective Action Plan (CAP) and often with at least two years of monitoring activity.
Have you ever doubted whether a small billing company or independent physician practice actually ever face penalties?
Well, keep in mind, a Business Associate is a ‘person’ or ‘entity’. This means that there is no billing company too small to have to comply with the Federal HIPAA regulations. Again, if you have not completed an accurate and thorough security risk assessment prior to that, you could also be penalized under ‘willful neglect’. This category alone is $50,000 per violation!
It is important for you to understand that every complaint or potential breach must be investigated by HHS/OCR. If you, a billing company, or another vendor suspects a breach, you must inform the covered entity (your client) and have a breach risk assessment completed to determine key factors and take action.
An EZClaim partner, Live Compliance, will help you to make checking off your compliance requirements extremely simple. They provide:
- Completely online, our role-based courses make training easy for remote or in-office employees.
- Contact-free, accurate Security Risk Assessments are conducted remotely. All devices are thoroughly analyzed regardless of location. Conducting an accurate and thorough Security Risk Assessment is not only required but is a useful tool to expose potential vulnerabilities.
- Complete set of HIPAA Policies and procedures built directly into your portal. Includes actionability, change management documentation, and Incident Response Policy to assist with your Corrective Action Planning. Easily share policies with staff with one click.
- Built directly into your portal, easily monitor where your workforce may be vulnerable with our Dark Web Breach Searches. Easily expose breach sources with ongoing searching of active employee email or domain ensuring continued awareness of potential breach exposure. Weekly automatic email notifications if new breaches are discovered.
- Short, informative, privacy awareness videos covering technical, administrative, and physical safeguards with topics such as ransomware, phishing, the Dark Web, password protection, and more. All delivered monthly with no logins required, they empower your workforce to make conscious decisions when it comes to your organization’s privacy and security.
So, don’t risk your company’s future, especially when Live Compliance is offering a FREE Organization Assessment to help determine your company’s status. For more information, visit their website, e-mail them, or give them a call at 980.999.1585.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call them today at 877.650.0904.
[ Contribution by Jim Johnson with Live Compliance ]