Nov 10, 2020 | Medical Billing Software Blog, Partner, Revenue, Support and Training, Waystar
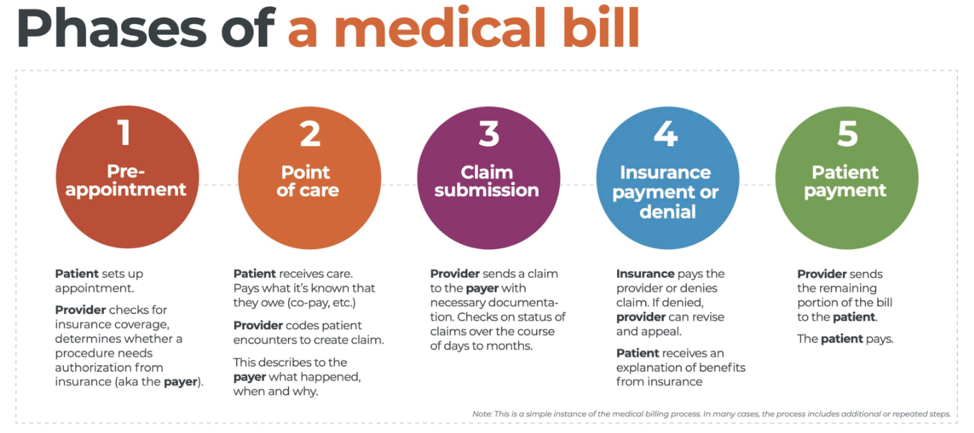
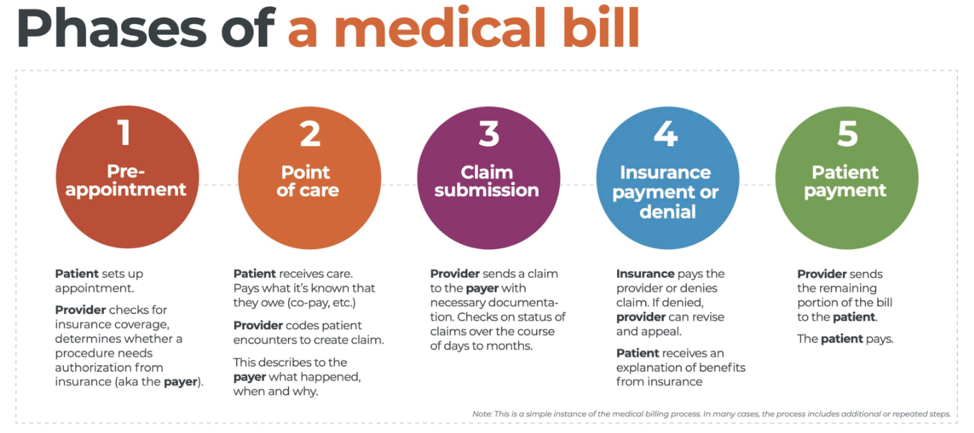 There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.
There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.
With high deductible health plans on the rise, the recent explosion of telehealth appointments due to COVID-19, and many other factors in play, it’s more important than ever for everyone to understand the life cycle of a medical bill, and how the process works. The healthcare revenue cycle is relevant not only to those who work in healthcare, but to the patient, too.
The revenue cycle is the series of processes around healthcare payments—from the time a patient makes an appointment to the time a provider is paid—and everything in between. One way to think of it is in terms of the life cycle of a medical bill. Although there are many ways this process can play out, this post will lay out a common example below:
1. Pre-appointment
For most general care, the first stage of the revenue cycle begins when a patient contacts a provider to set up their appointment. Generally this is when relevant patient information will begin to be collected for the eventual bill, referred to on the financial side of healthcare as a claim.
At this point a provider will determine whether the appointment and procedure will need prior authorization from an insurance company (referred to as the payer). Also, the electronic health record (EHR) used to help generate the claim is created, and will begin to accumulate further detail as the provider sends an eligibility inquiry to check into the patient’s insurance coverage.
2. Point of care
The next step in the process begins when the patient arrives for their appointment. This could include when a patient arrives for an initial consultation, an outpatient procedure, or for a follow-up exam. This could also include a Telehealth appointment.
At any of these events, the provider may charge an up-front cost. One example of this is a co-pay, which is the set amount patients pay after their deductible (if they are insured), however, there are other kinds of payments that fall into this category, too.
3. Claim submission
After the point of care, the provider completes and submits a claim with the appropriate codes to the payer. In order to accomplish that, billing staff must collect all necessary documentation and attach it to the claim. After submitting the claim to the payer, the provider’s team will monitor whether a claim has been been accepted, rejected, or denied.
[ Note: Medical coding refers to the clerical process of translating steps in the patient experience with reference numbers. The codes are normally based on medical documentation, such as a doctor’s notes or laboratory results. These explain to a payer how a patient was diagnosed and treated, and why. This information helps the payer decide how much of an encounter is covered under any given insurance plan, and therefore how much the payer will pay. ]
4. Insurance payment or denial
Once the payer receives the claim, they ensure it contains complete information and agrees with provider and patient records. If there is an error, the claim will be rejected outright and the provider will have to submit a corrected claim.
The payer then begins the review process, referred to as adjudication. Payers evaluate claims for accurate coding and documentation, medical necessity, appropriate authorization, and more. Through this process, the payer decides their financial obligation. Any factor could cause the payer to deny the claim.
If the claim is approved, the payer submits payment to the provider with information explaining details of their decision. If the claim is denied, the provider will need to determine if the original needs to be corrected, or if it makes more sense to appeal the payer’s decision.
Following adjudication, the payer will send an explanation of benefits (EOB) to the patient. This EOB will provide a breakdown of how the patient’s coverage matched up to the charges attached to their care. It is not a billing statement, but it does show what the provider charged the payer, what portion insurance covers, and how much the patient is responsible for.
5. Patient payment
The next phase occurs when the provider sends the patient a statement for their portion of financial responsibility. This stage occurs once the provider and payer have agreed on the details of the claim, what has been paid, and what is still owed.
The last step occurs when a patient pays the balance that they owe the provider for their care. Depending on the amount, the patient may be able pay it all at once, or they might need to work with the provider on a payment plan.
The above example represents one way the lie cycle of a medical bill can play out. Some of the ‘phases’ are often repeated. Because of the complexity of healthcare payments and the parties involved, there is not always a ‘straight line’ from patient care to complete payment. That’s why we call it the revenue cycle, and there are companies that provide systems for its management.
One of EZClaim’s partners, Waystar, aims to simplify and unify healthcare payments. Their technology automates many parts of the billing process laid out above, so it takes less time and energy for providers and their teams, and is more transparent for patients (Click here to learn more about how Waystar automates manual tasks and streamlines workflows.) When the revenue cycle is operating at its most efficient, providers can focus their resources on improving patient care—and that’s a better way forward for everyone!
For more information of how Waystar works together with EZClaim, click here.
[ Article and image provided by Waystar ]
———————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support, and can help improve medical billing revenues. To learn more, visit their website, e-mail them at sales@ezclaim.com, or call a representative today at 877.650.0904.

Nov 10, 2020 | Alpha II, BillFlash, Claims, collections, Denied Claims, EZClaim Premier, HIPAA, Medical Billing Software Blog, Revenue, Support and Training
It IS POSSIBLE to improve medical billing revenues, and here are a few ways to do just that.
Healthcare practitioners, whether established or just starting out, have many overwhelming tasks: Managing a practice; Seeing patients; Working to staying up-to-date on administrative tasks; The whole host of compliance at the federal, state, and local level; and Overseeing the billing.
One of these that can lead to loss of revenue is not properly managing the medical billing, which can also lead to HIPAA fines and rejected claims. However, there is a solution: a medical billing system that balances the budget and optimizes revenues of medical practice.
EZClaim, an expert in the medical billing software market since 1997, provides a solution that improves the efficiency of an office’s billing process in many ways. The following are the primary reasons.
Reduce Coding Errors
Medical procedures become codes, codes become claims, and claims become revenue. Any error in this process can make claims to be denied, your workload can be increased, and revenue can be lost. To help in avoiding errors, it is essential to use billing software that offers the easiest implementation and access to descriptive diagnosis and treatment codes. EZClaim’s medical billing solution offers ease-of-use in coding, billing, and strong partnerships with Clearinghouses which act as an additional ‘safety net’ for catching errors.
Administrative Support
Most medical practices are a small team of people tackling a wide range of tasks, so when one cannot understand the function of the billing software, accessing reliable support is very important. EZClaim prides itself on having dedicated support experts available, and that was how the company was established. Founder and President Al Nagy has said, since day one, “We are a support company that happens to sell medical billing software.”
Maintain Industry Compliance
It is important to recognize that industry compliance and a practice’s revenue go hand-in-hand. Filing and batching inaccurate and non-HIPAA compliant claims can often be traced back to an outdated healthcare revenue management system. Conquering these tasks requires a focus on multiple fronts: A properly trained billing team, clear office procedures, patient payment policies, and a reliable medical billing company. These are all ways to help buttress against non-compliance and rejected claims.
Streamline Workflow
Recently, a study was done that showed almost 80% of medical bills contain errors. These incorrect medical claims often end up as lost revenue originally, not to mention the additional cost of resubmissions and collections. One of the best ways to resolve this problem for your practice is to make use of both well-trained, experienced billers and coders, combined with a competent medical billing solution that aids in catching these errors. EZClaim software features a library of standard validation, the ability to add custom validation, and integrates with Alpha II for full claim scrubbing.
Follow up
Errors will and do occur, so establishing a system for follow-up on all denials will close the loop and protect against lost revenue. Being consistent with the follow-up process, and having a medical billing solution that tracks these things will help close that gap.
Collections
Finally, probably the most important aspect that optimizes a practice’s revenue is to get paid. Portals and payment collection systems definitely help with this, but having collections integrated into the medical billing system is, of course, the best. EZClaim has pain-free payment processing integrated into their solution, called EZClaimPay. It solves all the problems associated with payment processing: Bank deposits, reconciliation, statements, changing fees, and ‘finger-pointing’ when there is a problem. EZClaimPay’s robust platform will greatly increase a practice’s collections success, and improve their revenue.
———————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support, and can help improve medical billing revenues. To learn more, visit their website, e-mail them at sales@ezclaim.com, or call a representative today at 877.650.0904.
[ Photo credit: Studioarz ]


Oct 13, 2020 | Health eFilings, Webinar
This FREE Medicare reimbursements webinar will help healthcare providers with the financial challenges they are facing this year, and it’s critical not to ignore the impact MIPS compliance has on their bottom line.
There are many commonly misunderstood aspects of MIPS (Merit-based Incentive Payment System), and many nuances of how and when actions need to be taken to be able to earn points—and points significantly impact reimbursements!
To help bring clarity to MIPS, Health eFilings is holding a FREE 30-minute Medicare reimbursements webinar to help you understand key deadlines for this reporting period, what reporting methods will optimize your MIPS score, and how to increase the financial payouts from the MIPS program.
• Date: TUESDAY, DECEMBER 8, 2020, 1:00 – 1:30 pm EST
• Presenter: SARAH REITER, SVP Strategic Partnership of Health eFilings
• Register Here: https://healthefilings.com/ezclaim
The 2020 reporting period is quickly coming to a close, but there is still time to comply and avoid penalties. However, you must act quickly, so Health eFilings is here to help: https://healthefilings.com/ezclaim

Health eFilings is a ‘partner’ of EZClaim, a medical billing and scheduling software solution. For more details about their software, visit their website: ezclaim.com/features-pricing/
Oct 12, 2020 | Medical Billing Software Blog, Partner, Revenue, Waystar
Today’s healthcare landscape faces truly unprecedented challenges, which means it’s more important to get the most out of your analytics to develop more informed, strategic decisions. There’s a deep well of data that each revenue cycle feeds into, which if properly analyzed, can help organizations operate at their most efficient and effective. Here are the four stages of data analytics workflows that are key to developing those actionable insights: A “Trigger,” or the point in your revenue cycle that sets up the call for deeper analysis; “Interpretation” of data to determine root causes and identify appropriate next steps; “Intervention” to improve specific metrics; and “Tracking” of said metrics to chart success in achieving desired outcomes.
So, let’s examine what a successful version of each stage looks like:
Trigger:
The trigger occurs when you notice something that needs further investigation. With the right analytics tool you can easily access all of your key performance indicators, financial goals and more, providing the visibility you need into your rev cycle. When something looks amiss or needs improving, you can drill down to the level that shows what’s really going on.
Interpretation:
Even a wealth of data amounts to nothing without an efficient way to process and communicate key takeaways. You’ll need to equip your team with access to concise reports, smart visualizations and relevant historical data in order to get them to the insights that drive action.
Intervention:
Now is the time to take action. Intervention is ultimately tied directly to your ability to drill down into the data underlying problematic areas of your revenue cycle and clearly communicate takeaways with your team. Success at this stage depends on designing a plan based on your best understanding of underlying issues and the most effective way to address them.
Tracking:
Your intervention plan is built on KPIs that naturally intertwine with the way you measure success across your revenue cycle. With proper implementation and tracking, running with the analytics cycle can become a simple addition to your everyday workflow. More than delivering on your initial goals, the true power of analytics is the ability to deliver repeat value on your initial investment.
Wrap Up
A strong analytics solution does more than deliver a more fully developed picture of your revenue cycle performance. It provides actionable business intelligence, cuts down on time between analysis and action, and lessens the strain on your IT department.
Waystar is a ‘partner’ of EZClaim, and provides analytics for a practice using their medical billing software. For more details about EZClaim’s products and services, visit their website: https://ezclaim.com/
To learn more about how Waystar can help you harness the power of your data, call their main office at 844-4WAYSTAR, or call sales at 844-6WAYSTAR.
[ Contributed by Waystar ]

Sep 10, 2020 | Electronic Billing, Medical Billing Software Blog, Partner, Trizetto Partner Solutions
A group of senators introduced the “Health Care PRICE Transparency Act” in a move to empower patients to lower their healthcare costs.
On a basic level, the Act will require all medical facilities to post payer-negotiated rates for all shoppable services, so the patient can find the most inexpensive way to take care of their medical needs. This legislation will give Americans the chance to see the actual costs of their healthcare visits, which in theory, will increase competition and lower healthcare costs for everyone.
The added transparency of the Act will bring more accountability and competition to the healthcare industry, and gives American’s more control over their healthcare costs. However, if you are a medical practice, a hospital, or a member of the medical billing community, you need to know how you can best respond.
• “What is this procedure going to cost?”: There is going to be mounting pressure on practitioners, medical billers, and hospitals to have answers for the cost of procedures. Jeff Leibach, a director of Guidehouse’s healthcare strategic solutions team, says that “regardless of the legal fate of the final rule, hospitals need to be prepared for more price transparency in the future.” So, to get in front of this—and help you compete against your competitors—you should be prepared with both what it will cost for individual services and procedures, as well as, a ‘value statement’ on why it will cost what you are charging.
• Prepare to Comply or Cover the Costs: As it stands now, the legislation is moving towards technology assisting with the billing transparency. This will aid the patients to better understand the cost of services. This is a ‘clarion call’ for you to begin preparing for this reality or you will struggle with being fined and potentially publicly shamed in publications for being offenders. We recommend starting to comply NOW before the deadline ‘sneaks up’ on you.
• Use It To Improve: Currently, healthcare practices are, in many cases, already working at capacity. The added effort of defining cost and selling procedures are enough to make some healthcare facilities put this off until it is too late. Yet, while many may be considering accepting the fines and fees associated with non-compliance, we advise using this as an opportunity to improve—to better establish your medical practice’s services and promote your ability to be proactive to change. Getting ahead of the coming ‘wave’ of consumer expectations of healthcare will be a benefit.
• Seek Out Vendors That Can Assist: The changes that are coming for individual practices and healthcare providers can be overwhelming, and potentially it might just be more than what an IT team or private practice can handle. Forward-thinking billing departments should be investing in software vendors that can help fill that gap. EZClaim is a medical billing software company that partners with Trizetto to provide a tool called, Patient Responsibility Estimation (PRE). This tool assists in clarifying costs to consumers by providing a cheap and fast way for them to pay for out-of-pocket costs. [ Click here to learn more about how EZClaim can help you ].
It is clear that the expectations of consumers are changing, and the wave of medical transparency is on its way. Accepting it, preparing for it, and using vendor software to help overcome it, can be the difference of your practice avoiding fines and fees. For those forward-thinking and proactive practices who want to learn about how EZClaim can help, e-mail one of their sales representatives, go to their website for more details, or download a FREE 30-day trial today!
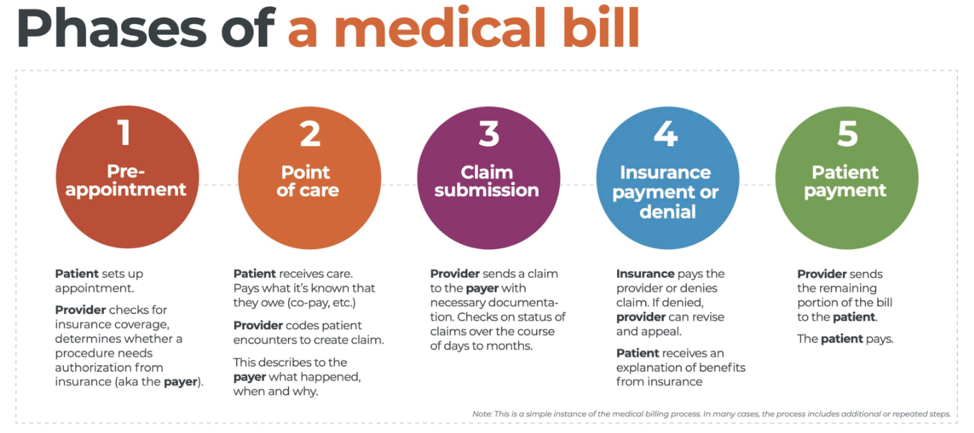
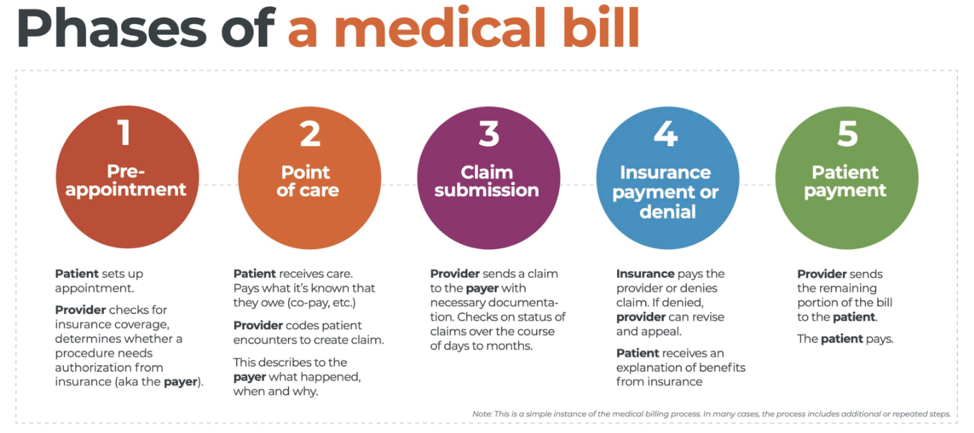 There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.
There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.