Sep 14, 2022 | EZClaim
As competition in the healthcare industry continues to heat up, providers and billers must look to new options to provide seamless and flexible payment options to retain customers and attract new ones.
Providing a variety of convenient payment options is more important than ever
Patients are frustrated by their healthcare payment options. While they understand the importance of paying their bills, they also want to be able to pay them in a way that is convenient. Many patients would rather pay their bills by credit card rather than cash or check, but they do not always have this option.
Patients have adopted a consumer mindset. From their perspective healthcare transactions should be no different from other transactions. They are more reluctant than ever to put a check in the mail and cross their fingers. In a world of easy online payments and tap-to-pay convenience, healthcare providers need to recognize that the patient financial experience is just as important as the patient care experience.
Most importantly, providing these payment options are not just about giving patients more convenience, but about the bottom line. Embracing new functionality like card-on-file recurring billing and SMS text message payment reminders saves your staff time and increases payment rates.
“We sent out the first SMS payment requests last week, and within several hours had generated 9 payments for a total of over $2,400 back from the patients! The provider is thrilled.”
As the healthcare industry continues to become more competitive, it becomes more critical than ever to create efficiencies wherever possible.
Patient payment data security must be a top priority
In 2016, healthcare organizations suffered a record-breaking number of data breaches. These breaches are not just affecting the health of patients and the financial bottom line of providers – they are also affecting their reputation.
A survey conducted by Ponemon Institute in 2017 revealed that healthcare organizations lost an average of $2.1 million per breach and nearly a third reported losing between $1 million and $10 million per breach. In addition to these costs, there are also significant reputational consequences for healthcare organizations that suffer a data breach. More than half (52%) said they would avoid using a provider following a data breach.
Consumers are concerned about safeguarding their medical information when paying bills; 47% have significant concerns regarding the security of making payments for both medical bills and health plan premiums. They want to take advantage of the consumer protection guarantees that their credit card company offers and a PCI compliant payment processing like EZClaimPay.
Finding the right payment processing partner
Healthcare is more complex than many other industries — a tangle of relationships between patients, healthcare providers, insurers, and unique regulatory requirements such as HIPAA. In this context, there are many providers find that their payment and billing systems do not work well together. Because of these challenges, medical billers and healthcare providers stand to benefit by working closely with their payment processors.
EZClaim set out to build a payment processor from the ground up that addresses these concerns. EZClaimPay helps billers and providers save time and money with functionality like card-on-file recurring billing, ability to offset processing costs with the platform fee functionality, and automatic reconciliation. Plus, increase payment rates with text message reminders and convenient payment portal. Most importantly, because we serve healthcare providers exclusively, we have ensured compliant, industry standard security including PCI compliance.
Streamlining and optimizing payment processing expedites the patient payment process while increasing back-office efficiencies. Healthcare providers that offer seamless, secure, and flexible billing and payment options will retain more customers and continue to attract new ones.
EZClaim is a leading medical billing, scheduling, and payment software provider that combines a best-in-class product with exceptional service and support. For more information, schedule a consultation today, email our experts, or call at 877.650.0904.
Aug 11, 2022 | EZClaim
The revenue cycle is a crucial component of a medical practice. Revenue Cycle Management (RCM) is the process of managing patient accounts, interacting with payers, processing claims, and collecting payments related to health care services. As the industry becomes more competitive and physicians are expected to perform more administrative tasks on their own, RCM has become even more important for healthcare providers today than ever before. Unfortunately, many practices still struggle with managing their RCM processes in an efficient manner that allows them to focus on what matters most: patient care. Below is a list of common mistakes made by healthcare providers when it comes to RCM.
Below is an overview of the seven key components of RCM and ways to avoid some of the most common mistakes.
Insurance Verification and Authorization
Insurance verification and authorization is a critical step in the revenue cycle process. If this step fails, all other steps must be repeated. This can result in delays, rework, denials of claims and even patient non-compliance.
- Verify that the patient is covered by their insurance plan and will not be responsible for additional costs related to their treatment or procedure (co-pay and deductibles).
- Verify that your provider is in network for each specific procedure with their chosen health plan/policy before completing any work on behalf of the patient.
- Ensure that all documentation supports your claim(s), including diagnosis codes and clinical notes from EMRs or doctors’ offices detailing what was performed during each visit. These details should align with those found on physical charts signed by both patients and providers alike.
- Verify eligibility rules as defined by health plans: has a deductible been met? Is there a copay amount due before benefits kick in? In some cases it may be necessary to contact members directly via phone or email asking them these questions so they know exactly how much they owe out-of-pocket. Our partner TriZetto Provider Solutions offers integrated eligibility verification. Automating this due diligence on the front end ensures that you are not left with the cost of having a biller redo this work, or worse, writing of claims.
Patient Registration and Copay Collection
Patient registration and copay collection are important first steps to ensure that your revenue cycle is functioning properly. Patient service, claims submission, remittance processing, and back-end patient collections are all vital components of the revenue cycle management process.
Without these steps in place, you will not be able to complete the full revenue cycle management process.
Service Coding and Charges
The service coding process identifies the type of service or procedure that was performed by your staff. Accurately documenting and coding charges allow you to:
- Assign appropriate codes for reimbursements from government programs, insurance companies and self-pay patients.
- Determine the level of reimbursement for each code
- Avoid fraud and abuse
Billing and Collections
It is critical to collect payments on time, in full and accurately. If you do so consistently, it will be easier to predict future cash flow needs and improve your ability to manage the revenue cycle.
Timely billing is critical because it allows the practice to collect their fees before they become delinquent. Delinquent accounts must be reported to credit agencies which can negatively impact a patient’s ability and willingness to pay for other services at your facility in the future. Late fees should also be considered for patients who are more than 60 days late paying their bill – this can help generate additional revenue by encouraging prompt payment from patients who may otherwise have ignored their bills altogether.
Accuracy is key when collecting payments because inaccurate claims may result in denied reimbursement by Medicare or third-party payers’ due out-of-pocket expenses for patients who were mistakenly overcharged by providers.
Consistency means that providers need regular updates on where each account stands within its cycle; this helps ensure that both patient satisfaction levels remain high and that everyone receives timely access. Efficiency refers not only to how quickly accounts move through management but also how quickly they get paid so providers know exactly how much money they’ll have coming in each month before making subsequent budgeting decisions.
EZClaim provides great tools to help ensure your collections are timely, accurate, and consistent. EZClaim allows you to keep a credit card on file. With approval to charge up to a specified amount, you can make it convenient for your patients and ensure payments are timelier than ever. EZClaimPay also offers email and SMS text message-based reminders, which have proven effective in increasing payment rates.
Denial Management
Denial management is the process of managing patient denials. Denials can be caused by a variety of reasons, including incorrect CPT codes, missing information, or provider errors. Therefore, it’s important to have ready-to-go processes for handling them and getting paid as soon as possible.
When you receive a denial from an insurance company, there are several things you should do immediately:
- Double-check that all your claims are accurate and complete before submitting them for payment. If there is any ambiguity on the part of the patient or their healthcare provider, this will increase the likelihood that your claim will be denied due to lack of clarity.
- Request that more specific details regarding the denial be provided. This allows better preparation when submitting future claims related to this patient’s care and ensures there aren’t additional denials for similar reasons.
The revenue cycle is a crucial component of any medical practice. It’s also one of the most challenging aspects of running a practice, especially in today’s increasingly complex environment. This article has highlighted some common mistakes that can be made when managing your revenue cycle and how to avoid them.

Jul 19, 2022 | EZClaim
Demand for different care models and emerging technologies are changing how healthcare is delivered in 2022. These are the trends to watch this year.
More Medical Technology Integration
Integrating medical technologies to broaden available data and improve patient outcomes will continue to impact the way hospitals, healthcare centers, and care providers operate. These new tools and integrations will allow healthcare professionals to use more efficient workflows thanks to better APIs and less data silos.
Integration means collecting more data with new remote monitoring and Medical “Internet of Things” devices. This data can then be centralized for patients and doctors with with cloud-based electronic health record platforms. It also means better patient education with consumer mobile apps, automated care-team emails and text messages, and digital therapeutics. These integrated tools will continue making it easier for doctors to collect and access more precise and detailed patient data than ever before.
As more technology works together, providers can identify and solve medical issues faster and more accurately. Further, patients are given opportunities to become more involved in achieving their healthcare goals and taking part in preventative measures.
Telehealth Continues to Grow
Today, many providers offer telehealth options to patients who prefer to meet with their doctor via phone or video. This option is one of the fastest growing in healthcare and will be an increasingly popular way to access healthcare in the coming years.
Telehealth can be beneficial for both providers and patients by lowering costs and increasing availability. Telemedicine allows healthcare providers to reduce their overhead and pass on those savings to patients by removing the need to visit a physical office. In addition, telehealth capabilities have made rural access easier by giving Americans a broader range of providers in different specialties. Traveling for healthcare can be expensive in terms of money and time. Virtual care offers lower costs, greater access to primary care for those in rural areas, and better public health.
The option to meet with a provider by phone or video is also a great tool to bring in and retain new patients. Lowering barriers to entry and establishing relationships via video or phone can be a great way to provide quality care initially and preserve that patient over the long term.
Healthcare consumerism was slowly growing before COVID, and patients see technology as a way to improve their mental and physical well-being. Telehealth will play a major role in those consumer expectations.
Home Health will Become More Popular
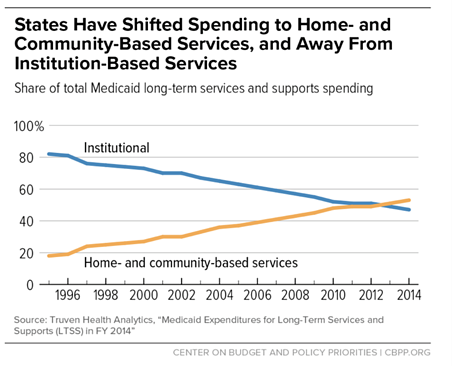
As more baby-boomers hit retirement age, demand for home health nurses and services—which were already seeing a surge in demand with COVID-19—will only continue to increase. As home health monitoring technology becomes increasingly available, states and private equity increases funding for these programs, and many seniors opt to return home instead of a skilled nursing facility, the trend towards home health is clear.
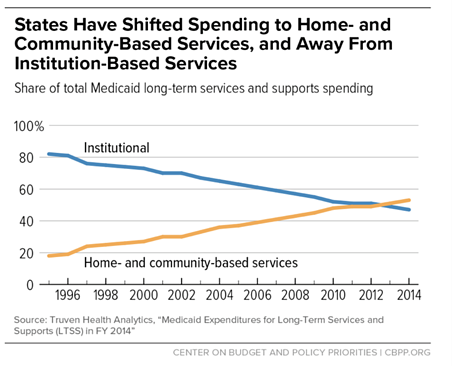
Medicare data reflects this trend as well with the Medicaid Innovation Accelerate Program reporting continued growth in home and community services.
Emerging technologies and care models are driving the way forward in 2022. These innovations will provide new ways for providers to deliver better care and more value to their patients.
EZClaim is a leading medical billing, scheduling, and payment software provider that combines a best-in-class product with exceptional service and support. For more information, schedule a consultation today, email our experts, or call at 877.650.0904.