Aug 11, 2020 | Medical Billing Software Blog
The most important thing a medical practice can do for their financial health is collecting payments from patients. So, because patients are not usually savvy when it comes to the nuts and bolts of their contract, they become frustrated when you send them a bill and, beginning on January 1st, your office staff get inundated with the question, “Why do I have a balance?”
“Approximately 68% of patients with bills of $500 or less did not pay off the full balance during 2016—up from 53% in 2015 and 49% in 2014.” Source: Patients May be the New Payers, But Two in Three Do Not Pay Their Hospital Bills in Full, TransUnion Healthcare, June 26, 2017
So, let’s make sure your office is equipped and able for collecting payments from patients for the services you rendered, rather than them becoming a part of this scary statistic.
Let’s begin with the basics: Make sure that your staff understands these key terms, and is comfortable explaining them to your patients.
Deductible: The deductible is the amount the patient has to pay for covered services before the insurance plan pays. Some insurance plans will apply an office visit to the deductible, others will not. Family plans typically have an individual and family deductible.
Copay & Coinsurance: These are both the portion the patient will be responsible for after their deductible has been met. Copays are a set, flat fee. Coinsurance is a set percentage that the patient will pay.
Maximum Out-of-Pocket: This is the limit of what a patient will pay for covered services within a plan year. Again, on family plans, there may be an individual max and family max.
Now, keep in mind that your staff will not know the details of your patients’ plans, nor should they be expected to! In the ever-changing world of health insurance, patients need to become better consumers. So, just being able to explain these key terms and why they create a patient balance will help them become better insurance plan shoppers!
Use your tools. Look into using Integrated Eligibility (available through your billing software and your clearinghouse). This will allow your staff to check remaining deductible balances, copay, and coinsurance amounts with the click of a button. These results allow practices to confidently collect at the time of service rather than spending time and money on sending statements and working to collect after the visit.
In addition to that, create a plan and stick to it. Use this time to review the efficiency of your patient collections plan. Are you using an outdated plan or policy? Have you considered offering payment plans to patients with an HSA card kept on file? Make sure that your employees understand how important patient collections are to the practice, educate them on the plan, and support them when they hold patients accountable to the patient collections policy.
For more information on how EZClaim can help you with this journey, schedule time with our sales team. Or, if you ready to get started right now, then download your FREE 30-day demo today!
[ Written by Stephanie Cremeans of EZClaim ]

Apr 13, 2020 | Medical Billing Software Blog, Revenue, Trizetto Partner Solutions
Because of COVID-19, some practices are doing triage from the car before they will allow a patient into their offices. Practices should also take a ‘cue’ from this by instituting protective measures for their finances.
I went to the doctor for a regular visit last week, which seemed anything but regular. I sat in the car and called to let them know I had arrived. They verified my demographics and insurance information over the phone; me in the parking lot, them in the office. The MA came out with her PPE and took my temperature, found me to be fever free so I could enter the building.
My nurse practitioner came in for our visit. We went about our appointment as usual except this time she took my superbill upfront herself and handed it to the check-out staff member. We scheduled a Telehealth visit instead of a traditional office visit. At the checkout desk, I said “I’m pretty sure I have a balance from the last visit, can I take care of that today?”. I loved where their heart is at, but I was sad to hear her say “You do, but we aren’t worried about that today. Just pay when you get the next statement.”
With so many things in chaos right now, so much thrown at you, and out of your control – let us not forget about the protective measures you can put in place for your practice. This is the time to get some vitals and triage from the car, before blindly allowing the chaos into your business. So, what should you be tracking?
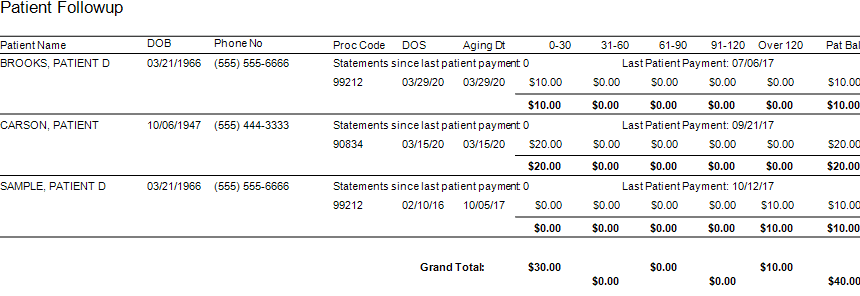
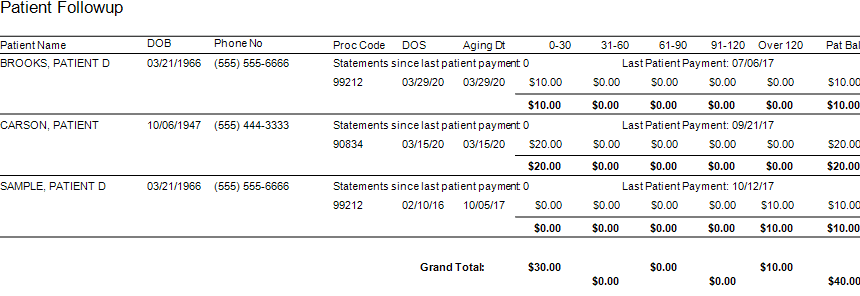
Start with basics – look at the aging balances. More than likely, you have money on the table! In EZClaim, you have the option to run full aging, but the more efficient option is running the Insurance Follow Up report and the Patient Follow Up report. Just running these reports will let you know where there is money that needs to be collected. In addition – it just may show you that it is time to reevaluate policies and procedures in your office related to patient balances and insurance follow-up. Here is a peek at what these two reports can do for you.
Patient Follow Up Report: This report will show you balances that are outstanding with your patients. While this may not be the easiest time to ask patients to pay their balances, there are steps you want to consider:
- Consider what you will do with lingering patient balances. The Patient Follow Up report will show how many statements have been sent since the last patient payment. If you have sent several statements is it worth continued efforts?
- Contact your patients to see if they can pay with an HSA or FSA account
- Offer to set up a payment plan
- Write off the balance as a bad debt or a one-time professional courtesy
- Consider sending the account to collections
- Use technology to your advantage. Take this time to consider enabling online payment options.
- Create or revise patient payment policies and train your staff on these policies
Insurance Follow Up Report: This report will show your balances that are outstanding with insurance companies. Some of the useful features of this report include:
- Ability to see the aged balances by the payer. This lets you get the biggest bang for your buck. Look for payers that have a large percentage of balances in the oldest buckets and work those first.
- All the information you need for calling the insurance is right there on the report. You will have easy access to the date of birth, member ID number, and claim totals on the report.
- During your research, you will find common themes. Use these themes to update your office procedures and train your staff to eliminate errors so that claims get paid quicker.
EZclaim billing software can help you manage your office’s finances. Visit our website to find out more about our solutions: https://ezclaim.com/
[ Contribution by Stephanie Cremeans with EZClaim ]