Apr 13, 2020 | Live Compliance, Medical Billing Software Blog, Partner
Since CMS HHS just updated their Telehealth regulations to adjust to the COVID-19 environment—including having a remote workforce—we wanted to provide a clear update to independent physicians and billers to advise them of the fast-moving changes of many regulations, and what to expect in the near future.
It is important to note that CMS has recently announced that new and established patients have availability to Telehealth, and HHS OIG is providing flexibility for healthcare providers to reduce or waive cost-sharing for Telehealth visits paid by federal healthcare programs. CMS is also expanding Telehealth services to people with medicare.
As a result, please see the below video from CMS which highlights the Medicare Coverage and Payment of Virtual Services and Telehealth.
In addition, we’ve included a few key questions and answers below. If you have further questions about Telehealth and your compliance, contact Jim Johnson with Live Compliance at Jim@LiveCompliance.com or (980) 999-1585.
1. Who can provide Telehealth services?
-
- Physicians
- Nurse Practitioners
- Physician assistants
- Nurse-midwives
- Certified nurse anesthetists
- Clinical psychologists
- Registered dietitians
- Nutrition professionals
2. What services can a medicare beneficiary receive through Telehealth?
-
- Evaluation and management visits (common office visits)
- Mental health counseling
- Preventive health screenings
- More than 80 additional services
3. What are the types of virtual services?
-
- Medicare Telehealth visits
- Virtual check-ins
- E-visits
- Telephone services
Live Compliance is an EZclaim premier partner for HIPAA compliance and is integrated into EZclaim’s billing solution.
If you have any further questions about Telehealth regulations and your compliance, e-mail Jim Johnson at Live Compliance at Jim@LiveCompliance.com, or phone him at (980) 999-1585.
[ Contribution by Jim Johnson with the Live Compliance ]

Apr 13, 2020 | Medical Billing Software Blog, Revenue, Trizetto Partner Solutions
Because of COVID-19, some practices are doing triage from the car before they will allow a patient into their offices. Practices should also take a ‘cue’ from this by instituting protective measures for their finances.
I went to the doctor for a regular visit last week, which seemed anything but regular. I sat in the car and called to let them know I had arrived. They verified my demographics and insurance information over the phone; me in the parking lot, them in the office. The MA came out with her PPE and took my temperature, found me to be fever free so I could enter the building.
My nurse practitioner came in for our visit. We went about our appointment as usual except this time she took my superbill upfront herself and handed it to the check-out staff member. We scheduled a Telehealth visit instead of a traditional office visit. At the checkout desk, I said “I’m pretty sure I have a balance from the last visit, can I take care of that today?”. I loved where their heart is at, but I was sad to hear her say “You do, but we aren’t worried about that today. Just pay when you get the next statement.”
With so many things in chaos right now, so much thrown at you, and out of your control – let us not forget about the protective measures you can put in place for your practice. This is the time to get some vitals and triage from the car, before blindly allowing the chaos into your business. So, what should you be tracking?
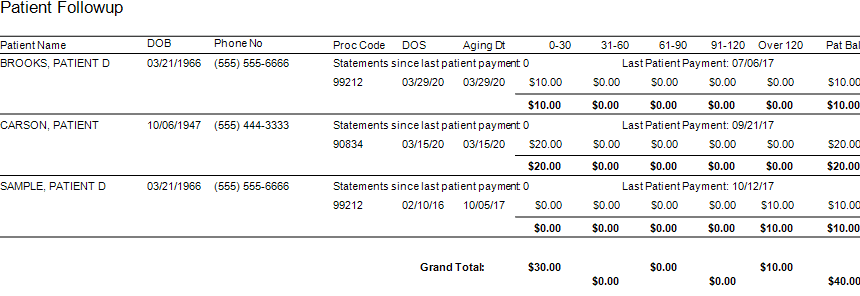
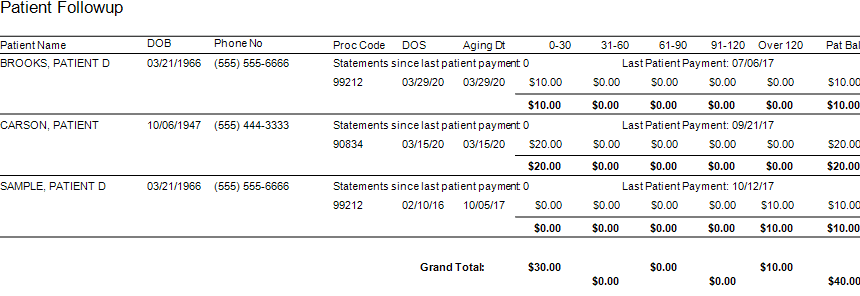
Start with basics – look at the aging balances. More than likely, you have money on the table! In EZClaim, you have the option to run full aging, but the more efficient option is running the Insurance Follow Up report and the Patient Follow Up report. Just running these reports will let you know where there is money that needs to be collected. In addition – it just may show you that it is time to reevaluate policies and procedures in your office related to patient balances and insurance follow-up. Here is a peek at what these two reports can do for you.
Patient Follow Up Report: This report will show you balances that are outstanding with your patients. While this may not be the easiest time to ask patients to pay their balances, there are steps you want to consider:
- Consider what you will do with lingering patient balances. The Patient Follow Up report will show how many statements have been sent since the last patient payment. If you have sent several statements is it worth continued efforts?
- Contact your patients to see if they can pay with an HSA or FSA account
- Offer to set up a payment plan
- Write off the balance as a bad debt or a one-time professional courtesy
- Consider sending the account to collections
- Use technology to your advantage. Take this time to consider enabling online payment options.
- Create or revise patient payment policies and train your staff on these policies
Insurance Follow Up Report: This report will show your balances that are outstanding with insurance companies. Some of the useful features of this report include:
- Ability to see the aged balances by the payer. This lets you get the biggest bang for your buck. Look for payers that have a large percentage of balances in the oldest buckets and work those first.
- All the information you need for calling the insurance is right there on the report. You will have easy access to the date of birth, member ID number, and claim totals on the report.
- During your research, you will find common themes. Use these themes to update your office procedures and train your staff to eliminate errors so that claims get paid quicker.
EZclaim billing software can help you manage your office’s finances. Visit our website to find out more about our solutions: https://ezclaim.com/
[ Contribution by Stephanie Cremeans with EZClaim ]

Apr 13, 2020 | BillFlash, Partner
Medical billing managing collections during COVID-19 will be different than it was in the past. It has already changed a lot about how medical practices operate, and in a short amount of time. One thing that hasn’t changed, however, is that practices need to get paid in order to continue operating. This includes sending patients to collections when necessary.
Managing late or unpaid bills during economic uncertainty may require a different approach than you’re used to. Before you send patients to collections, make sure you take these steps first.
- Be upfront about payment expectations from the beginning
-
- You should already have a strategy in place regarding informing patients how much they owe for services. Stick to it. Many people are hoping for leeway on certain bills due to the economic impact of COVID-19, but gently remind your patients that for essential healthcare services to continue, practices need to keep revenue flowing, and that means billing will continue as usual.
- Set up payment plans
-
- If a patient is unable to pay a bill in full, help them set up a payment plan. BillFlash PlanPay lets you set up scheduled, automatic payments to be paid over a set period of time. This is the best option for both you and the patient because:
- The patient has a more manageable bill
- Your practice is more likely to be paid in full
- Setting up a payment plan shows your patients you’re willing to work with them. That’s usually all they need to be assured that you care.
- Send out multiple reminders
-
- Use whatever resources you have—email, phone, text, mail—to contact patients about balances they owe. Be courteous in your reminders, but firm. Most patients want to pay their medical bills. Often all they need is a simple reminder and an easy way to make the payment.
- BillFlash helps you manage all of this during the pre-collections phase to help ensure you are paid as quickly and completely as possible.
If none of these steps work, then it’s time to get collections involved.
What to Include in a Collections Letter
Include all the facts of the visit. This includes:
-
- Date of service
- Service provided
- Amount patient owes
- Payment options
Tone of the Letter
The right tone in your letter can do more to ensure payment and a continued relationship with the patient than anything else you include. You need to convey a sense of urgency, but without being overbearing and intimidating.
A few tips to keep in mind:
-
- Empathize with the patient. Simply saying “We understand you may be experiencing financial difficulties at this time” is more likely to get a response than a curt “final warning” threat.
- Explain why it is important for the patient to pay anyway. Example: Like any other business, our practice relies on revenue to thrive. In order to continue to provide these valuable healthcare services, patients need to pay their bills in full and on time.
- Offer a payment plan. Give patients one more opportunity to pay their bills in smaller chunks over a period of time to avoid having their accounts sent to collections.
We’re all experiencing difficulties during this global pandemic. The only way to get through it is to work together. Being upfront with patients about payment expectations and being willing to work with patients who have fallen on hard times will help all of us through this global health crisis.
BillFlash Collections Services can help you in managing collections during COVID-19, and simplify and streamline all your other collection processes for you, saving you the headache of exporting, importing, and working with a disconnected agency.
As an EZclaim ‘preferred’ partner, BillFlash is fully integrated with the EZclaim Premier billing application. For more details, view this informational video: https://www.rcm.billflash.com/ezclaim For more information about the EZclaim billing solution, view our website: https://ezclaim.com/
Apr 13, 2020 | Health eFilings, Partner
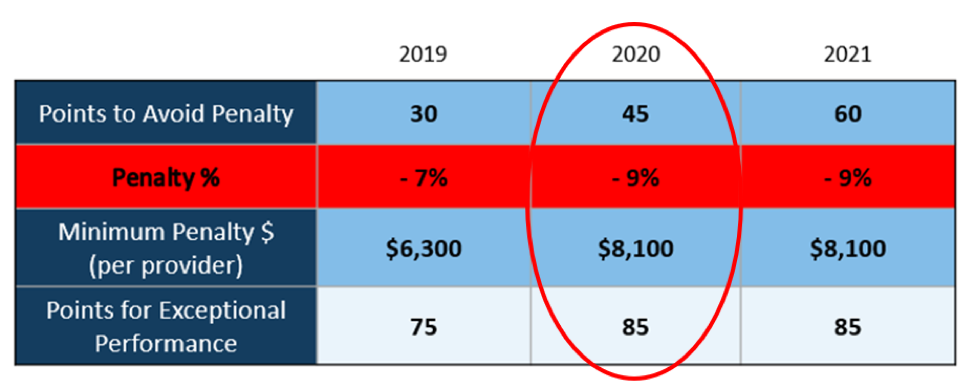
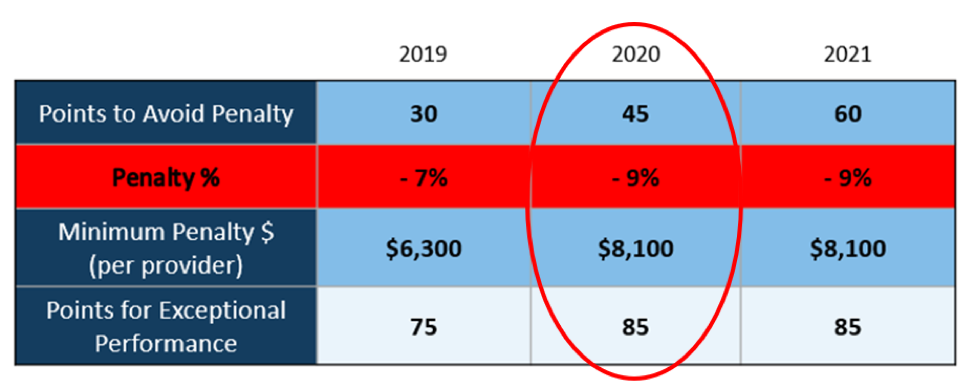
There WILL NOT be any changes to the MIPS Program in 2020, so all payers must be submitted and a minimum of 45 points must be earned to avoid the 9% penalty.
On March 23, 2020, CMS made it perfectly clear that MIPS Program is not going away in 2020. It also reiterated that the data requirements and thresholds in place for the 2020 program have not changed. Additionally, Promoting Interoperability and Improvement Activities must be done for the required durations, or no points will be earned for those categories.
To put this in context, while the stakes have been raised every year, the final ruling for the 2020 reporting period is the most complex to-date, further increasing the stress, burden, and financial risk for over 900,000 clinicians who bill Medicare Part B. Failure to comply or earn enough points for the 2020 reporting period will result in an automatic 9% penalty on every Medicare Part B claim paid for an entire year. This equates to a minimum of a $8,100 per provider hit to the bottom line.
Given the unprecedented time when everyone’s bottom line is at risk, now is the time to get a handle on what’s at risk with the MIPS program and proactively engage to ensure your bottom line is not further jeopardized by being assessed a 9% penalty. It can be challenging to know exactly what you need to do to earn points, optimize your score, and protect your Medicare reimbursements, as there are many commonly misunderstood aspects and nuances with the MIPS program.
So, with what is at stake and the inherent complexity in earning points, it is critical that you select the right methodology and partner who can help you maximize reimbursements and protect your bottom line. Not all reporting methodologies are the same.
Health eFilings‘ CEHRT is the best choice for a reporting partner. Their cloud-based ONC-certified software fully automates the process and does all the work without any IT resources, administrative support, and workflow changes from the practice. Health eFilings service is an end-to-end electronic solution that will save significant time, be a turn-key submission process, and maximize the financial upside for providers.
As more than 25% of the 2020 reporting period is behind us, now is the time to act while there is still plenty of time to positively impact your results and points earned.
Health eFiling provides the nation’s only fully automated solution for MIPS compliance and is integrated with EZclaim’s billing solution. Click on the following link for more details: https://healthefilings.com/ezclaim
[Contribution by Sarah Reiter with the Senior VP of Strategic Partnerships]
Mar 10, 2020 | Live Compliance, Medical Billing Customer Service
Whether you are a person new to medical billing or someone who’s been in the business for years, launching a new medical billing practice can be hard. Understanding the market, connecting with new clients, and knowing how to master your processes are challenges that you often learn as you go. Despite these challenges, it is rewarding to be out on your own growing a new company. Before you jump, let us help you understand some essential keys that you can research upfront and prepare yourself to get one step closer to being successful.
1. ONE BILLING PLATFORM VERSUS MULTIPLE PLATFORMS: First and foremost you must make a conscious decision to either focus on being an expert on an individual medical billing platform, like EZClaim or tackling multiple platforms. There are pros and cons of both: being an expert can make you extremely efficient in your use of the software’s billing and, scheduling features, however, it can also limit your client base to only one set of software users. Whereas having a basic understanding of multiple platforms can allow you a larger base of medical offices while limiting your ability to truly understand how best to serve each individual client’s needs.
Pro tip: Start and master one trusted billing program, and grow your options as your billing business grows.
2. GET CLEAR ON THE CLEARINGHOUSE: A new billing company owner does not want to be held to just one clearinghouse as options are key here. Having the ability to work with any or many would be an essential piece to your billing services, however, you still want to know the best clearinghouses in the business. Understanding which clearinghouses provide the best products and services and being able to recommend those services to your client upfront will make your life easier and their business run smoother. For this very reason, EZClaim has built its software around partnerships and integrations with the best clearinghouses to make working with the one you need easy.
3. COMPLY OR DIE (HIPAA Compliance): The third key to any start-up is first understanding the importance of HIPAA Compliance. Medical billing firms literally can come crashing down with any missteps, mistakes, or misunderstandings of this essential piece of the puzzle. It goes without saying that if you are going to choose a billing software be sure that they have partnerships built around making sure you are protected. You are also responsible to make sure the data is protected so your customer and their patient’s data is safe.
HIPAA Hint: Check out Live Compliance for further details on the topic.
There are many options available out there for your new medical billing practice, and we recommend doing your research. Within that research, you will find that EZClaim ranks very high in performance and comes in at a great price.
To learn about EZClaim go to our about page, sign up for a demo, and/or download a trial for free today!