Jan 15, 2022 | EZClaim
As we move into the new year, we wanted to take a moment to share the most popular articles of 2021. We’ve ranked them below so that you can be sure that you haven’t missed out on any resources that EZClaim clients have found useful in the past year.
Here are the most popular blog posts of 2021:
This interview was by far and away the most popular blog post over the past year. Jennifer and Maura provide some great insight and best practices, including their “investigative” approach to medical billing and the problem-solving skills that are necessary. Here is a summary of that article:
Are you working in the medical billing industry as a biller or an owner of a billing company? If so, the key medical billing insights and best practices that came out of our interview with Maura Jansen (VP of Operations) and Jennifer Withington (Director of Revenue) at Missing Piece Billing & Consulting Solutions will be very valuable for you to consider.
Jennifer, an expert in understanding the problem-solving techniques and the investigative nature of medical billing, offers insights that both educate and inspire. Maura, an executive member of the billing community, also added an important perspective about EZClaim’s medical billing software. The following are some highlights from our interview.
Getting patient billing information quickly can be a big pain point, so it makes sense that this article was among the most read of the year. We walked through some tips and ticks for saving time including the EZClaim eligibility feature:
Can you add up the number of hours your billing team spent during any given week or month waiting on-hold with insurance companies to get patient billing information? Does your staff invest hours of their valuable time seeking out the smallest of details to get paid? Are you aware that integrated eligibility, through EZClaim’s medical billing software, can reduce that time on-hold to a fraction of the total?
It is estimated that the average biller can spend up to 2-hours on-hold just to get an insurance company on the phone. Add to that an average of 10 – 15 minutes to talk through a patient and most companies will only address one or two patients at a time.
In this interview with a medical billing expert and co-owner of Elite Billing Resolutions, Vicky Greenwood, we talk about dealing with the challenges in owning a billing company, some important skills that every medical biller needs, and the value of choosing the right medical billing software. In our time speaking with Vicky, we focused on topics that will aid, contribute, and help grow the skills of the medical billing community. We at EZClaim believe in highlighting the best practices in the industry and sharing those with the larger community. We encourage you to consider these insights, and then let us know what topics you would like to learn more about.
Double data entry is frustrating. Luckily there is a better way—integrating your EHR with EZClaim.
Are you or your staff having to enter every patient into your EHR program and then again into EZClaim? There is an easier way! Integrating your programs will put an end to duplicate data entry, saving your practice time and money!
So, what exactly is an interface and how does it work? An interface is a way for two programs to share information. For EZClaim clients, the interface can be set up to share data from your EHR program to EZClaim. Your EHR can give you specifics on how to send the data to EZClaim.
Minimizing and preventing claim denials is a challenge that providers are increasingly running up against. We put together four strategies to address this growing problem:
Reducing claim denials has long been a challenge for providers. In the worst case, denied claims end up as unexpected—and sometimes unaffordable—bills for patients. The challenge only seems to be growing. A recent survey conducted by the American Hospital Association (AHA) found that 89% of respondents had seen a noticeable increase in denials over the past three years, with 51% describing the increase as “significant.”
Minimizing loss will be top of mind for providers as the COVID-19 pandemic continues to put a strain on their resources, and minimizing or preventing denials will need to be a core part of that strategy. With that in mind, we’re offering four tips to help guide revenue cycle strategies for better denial reduction in 2021.
There you have it, the most popular posts on the EZClaim blog in 2021. We look forward to keeping you up to date on everything medical billing in the new year!

Nov 24, 2021 | EZClaim
In a post-2020 world, consumers now expect every purchase and transaction they make to be personalized, digital, and simple. Groceries can be delivered and paid for with one click of a button. You can try on clothing virtually, get fitted for glasses, and even visit your doctor through your mobile device. To remain competitive, consumer-driven industries have had to create new and innovative ways to engage customers.
The healthcare industry has seen this shift as patients are behaving more like consumers in their healthcare interactions. Switching to a customer-centric mindset can be tricky for the healthcare industry as balancing patient communication and adhering to HIPAA and other regulations is essential. However, these new expectations have opened the door for the medical billing industry to innovate and move forward.
For the medical billing industry, consumers are asking for simplicity and convenience, but they still want choices. According to Healthcare Finance, fewer patients are paying their medical bills by check as the shift to online payment accelerates. It is important for the medical billing industry to understand that while a large segment of older Americans still pays bills through the mail, in-person, or by check, there are growing numbers of patients who prefer an online and mobile bill payment option.
As a solution to the ever-changing environment of payment reconciliation, in 2020 EZClaim launched EZClaimPay with the following features:
-
- Allows medical staff to text and email patients with payment reminders
- Allows patients to make payments on their mobile devices or online
- Save credit cards online for fast easy patient payments
- Gives patients the ability to save and print their own receipts
- Patient payments made online import directly to your EZClaim Billing program
- Collect payments 24-hours a day with no change to your “schedule”
In a rapidly changing world that is becoming more technology-based, the medical billing industry must keep up with current consumer trends. EZClaimPay is an excellent tool to keep your practice cutting edge and offers your patients the latest in bill-paying options.
ABOUT EZCLAIM:
As a medical billing expert, EZClaim can help the medical practice improve its revenues since it is a medical billing and scheduling software company. EZClaim provides a best-in-class product, with correspondingly exceptional service and support. Combined, EZClaim helps improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.

Apr 13, 2020 | Medical Billing Software Blog, Revenue, Trizetto Partner Solutions
Because of COVID-19, some practices are doing triage from the car before they will allow a patient into their offices. Practices should also take a ‘cue’ from this by instituting protective measures for their finances.
I went to the doctor for a regular visit last week, which seemed anything but regular. I sat in the car and called to let them know I had arrived. They verified my demographics and insurance information over the phone; me in the parking lot, them in the office. The MA came out with her PPE and took my temperature, found me to be fever free so I could enter the building.
My nurse practitioner came in for our visit. We went about our appointment as usual except this time she took my superbill upfront herself and handed it to the check-out staff member. We scheduled a Telehealth visit instead of a traditional office visit. At the checkout desk, I said “I’m pretty sure I have a balance from the last visit, can I take care of that today?”. I loved where their heart is at, but I was sad to hear her say “You do, but we aren’t worried about that today. Just pay when you get the next statement.”
With so many things in chaos right now, so much thrown at you, and out of your control – let us not forget about the protective measures you can put in place for your practice. This is the time to get some vitals and triage from the car, before blindly allowing the chaos into your business. So, what should you be tracking?
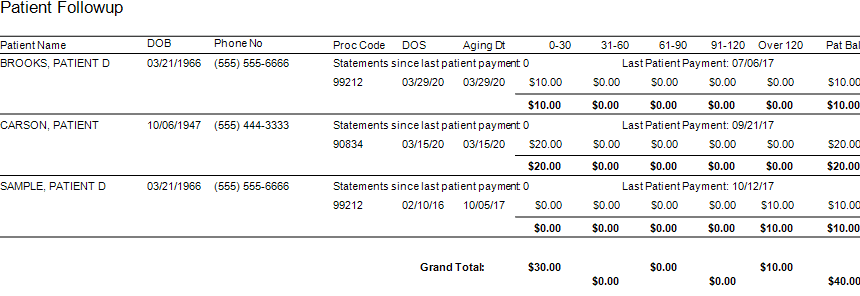
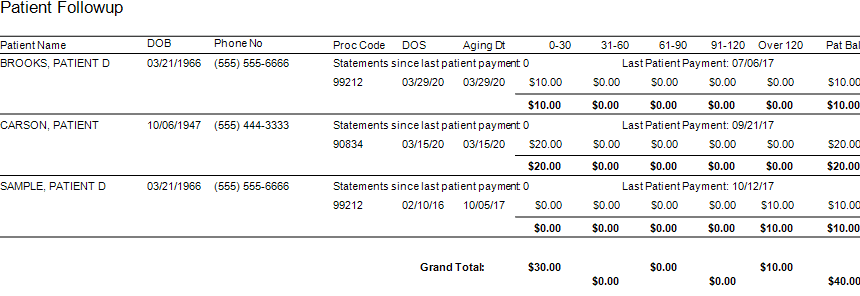
Start with basics – look at the aging balances. More than likely, you have money on the table! In EZClaim, you have the option to run full aging, but the more efficient option is running the Insurance Follow Up report and the Patient Follow Up report. Just running these reports will let you know where there is money that needs to be collected. In addition – it just may show you that it is time to reevaluate policies and procedures in your office related to patient balances and insurance follow-up. Here is a peek at what these two reports can do for you.
Patient Follow Up Report: This report will show you balances that are outstanding with your patients. While this may not be the easiest time to ask patients to pay their balances, there are steps you want to consider:
- Consider what you will do with lingering patient balances. The Patient Follow Up report will show how many statements have been sent since the last patient payment. If you have sent several statements is it worth continued efforts?
- Contact your patients to see if they can pay with an HSA or FSA account
- Offer to set up a payment plan
- Write off the balance as a bad debt or a one-time professional courtesy
- Consider sending the account to collections
- Use technology to your advantage. Take this time to consider enabling online payment options.
- Create or revise patient payment policies and train your staff on these policies
Insurance Follow Up Report: This report will show your balances that are outstanding with insurance companies. Some of the useful features of this report include:
- Ability to see the aged balances by the payer. This lets you get the biggest bang for your buck. Look for payers that have a large percentage of balances in the oldest buckets and work those first.
- All the information you need for calling the insurance is right there on the report. You will have easy access to the date of birth, member ID number, and claim totals on the report.
- During your research, you will find common themes. Use these themes to update your office procedures and train your staff to eliminate errors so that claims get paid quicker.
EZclaim billing software can help you manage your office’s finances. Visit our website to find out more about our solutions: https://ezclaim.com/
[ Contribution by Stephanie Cremeans with EZClaim ]