Jun 15, 2021 | Claims, Credit Card Processing, Medical Billing Customer Service, Medical Billing Software Blog
Are you or your staff having to enter every patient into your EHR program and then again into EZClaim? There is an easier way! Integrating your programs will put an end to duplicate data entry, saving your practice time and money!
So, what exactly is an interface and how does it work? An interface is a way for two programs to share information. For EZClaim clients, the interface can be set up to share data from your EHR program to EZClaim. Your EHR can give you specifics on how to send the data to EZClaim.
In EZClaim you will have an opportunity to review the file prior to saving the data. When you complete the import process, your claims will be created, and libraries will be updated. In addition to creating your claims for each visit, an interface can also create Physician/Facility library entries, as well as Payer library entries, and create new or update existing patient accounts.
If you are working with one of our partner EHRs (Visit our Partner List) the integration between programs can be set up quickly and easily. Since the process varies slightly depending on the EHR you are using, time to complete the integration request will vary.
If you are not using a partner EHR, you may still be able to integrate with EZClaim.
Following are some options:
- In our Online Help File the format types and specifications are available for you to share with your EHR vendor. If they can provide a file in one of the required formats you will be able to import your data.
- You may consider using a third party to write a custom interface for you. If you would like more information on this, contact EZClaim and we will be happy to provide information on consultants who are familiar with the EZClaim platform.
If you have questions, please submit them via email to support@ezclaim.com so a technician can review them and get back with you.
May 18, 2021 | Denied Claims, RCM Insight
Last month we looked at tools for getting clean claims out the door on the first try. Many billers or practices stop monitoring claims once the leave the practice management program, but this is where you are likely losing money. The unfortunate truth is you need to use the tools available to you to catch rejected and denied claims to ensure proper and timely payment. Today we will look at rejections and denials, and the resources you have (or need) to work efficiently.
The terms rejection and denial are used interchangeably in the billing world but they have distinct differences, including how you are notified. Let’s start with defining the differences.
Rejected Claims
- Claims can be rejected by the clearinghouse OR the payer
- Rejections are based on submission guidelines
- Rejected claims have not been entered into your payers system for adjudication
- Notified through a claim status report (ANSI 277) that comes back into most practice management programs from the clearinghouse
- Corrections do not require a resubmission code
Denied Claims
- Claims are denied by your payer
- Denials are based on policy coverage
- Denials have been accepted for adjudication and deemed unpayable
- Notified on remittance advice (ANSI 835/ERA)
- Payers may require a resubmission code and original reference number when submitting a corrected claim
If you are using a clearinghouse and receiving your claim status reports electronically, you will be notified quickly about rejected claims. There are two ‘checkpoints’ that will look for errors. The first is your clearinghouse, the second is the payer.
At each checkpoint claims will be Rejected or Accepted, these status updates come to you through a claim status report. If your practice management system is able to process these reports (ANSI 277) your claims will be updated with the accepted or rejected information you will be able to correct any rejected claims within your practice management system. When you see an error, start with checking who has rejected your claim. This will be the point of contact if you have questions about the rejection or how to correct it. If you are not already, make it a daily task to get your reports, correct any rejected claims, and resubmit those claims.
When a claim has been accepted by your clearinghouse and the payer it enters the adjudication system. This is where the payer will make a determination on payment based on the members coverage and your contract. The denials will appear on your remittance advice with a payment or as a zero dollar payment, indicating that they have reviewed your claim and they have determined no payment is applicable. If you are enrolled with you payer for electronic remittance advice (ERA) this file will come electronically and your practice management system will be able to list or identify denied claims. These claims will either need to be researched further for clarification on the denial or written off. It is vital that your practice management system can handle these scenarios appropriately so you do not lose money for payable services.
This is another scenario where technology can seem scary. However, efficiently monitoring and working is well worth the learning curve. If you are already sending electronically and not using the claim status report or electronic remittance advice – coordinate with your clearinghouse and practice management system to find out how these reports can save you time and money.
If you would like more information on creating workflows for rejections, denials, or enrolling with a clearinghouse, let RCM Insight help! Visit us at www.rcminsight.com to request a consultation.
[Contribution by Stephanie Cremeans with RCM Insight]
May 13, 2021 | HIPAA, Live Compliance
It’s no secret that the Dark Web is a scary place to lose your information, but what if it affected your entire company? Medical Records information sells anywhere from $1-$1000 by identity thieves!
What is a “breach” and where has the data come from?
A “breach” is an incident where data is inadvertently exposed in a vulnerable system, usually due to insufficient access controls or security weaknesses in the software. Data breaches are becoming more common and sometimes out of your control.
How can you protect yourself and/or your organization?
- Carefully monitoring where you store and enter your passwords can be extremely beneficial to help minimize the risk of a hack and keeping personal or patient information protected.
- Routine password changes and monitoring where you store and enter your passwords, can be extremely beneficial to help reduce the risk of becoming a victim to a hacker. Passwords should be long, unique in characters, capitalization, and alphanumerical.
If you believe you might have revealed sensitive information about your organization, report it to the appropriate people within the organization, including network administrators. They can be alert for any suspicious or unusual activity.
Firefox Monitor says, “Your password is your first line of defense against hackers and unauthorized access to your accounts. The strength of your passwords directly impacts your online security.”
Live Compliance can help. Live Compliance aggregates breaches and enables you to assess where their personal data has been exposed. Dark Web scanning is built right into the Live Compliance portal. Keep an eye on employees whose information was involved in a breach (and where the breach took place), and the suggested next steps to take.
What can I do to ensure this doesn’t happen to me or my organization?
At Live Compliance, we make checking off your compliance requirements extremely simple.
- Reliable and Effective Compliance
- Completely online, our role-based courses make training easy for remote or in-office employees.
- Contact-free, accurate Security Risk Assessments are conducted remotely. All devices are thoroughly analyzed regardless of location. Conducting an accurate and thorough Security Risk Assessment is not only required, but is a useful tool to expose potential vulnerabilities, including those such as Password Protection.
- Policies and Procedures curated to fit your organization ensuring employees are updated on all Workstation Use and Security Safeguards in the office, or out. Update in real time.
- Electronic, prepared document sending and signing to employees and business associates.
Don’t risk your company’s future, especially when we are offering a free Organization Assessment to help determine your company’s status. Call us at (980) 999-1585, or email me, Jim Johnson at Jim@LiveCompliance.com or visit www.LiveCompliance.com
For more information about DarkWeb breaches please contact us at (980) 999-1585 or email us at support@livecompliance.com
[Contribution by Jim Johnson at Live Compliance]

May 11, 2021 | Features, Medical Billing Software Blog
Can you add up the number of hours your billing team spent during any given week or month waiting on-hold with insurance companies to get patient billing information? Does your staff invest hours of their valuable time seeking out the smallest of details to get paid? Are you aware that integrated eligibility, through EZClaim’s medical billing software, can reduce that time on-hold to a fraction of the total?
It is estimated that the average biller can spend up to 2-hours on-hold just to get an insurance company on the phone. Add to that an average of 10 – 15 minutes to talk through a patient and most companies will only address one or two patients at a time. To add to it often there are multiple insurance companies to call. As you can tell you quickly have a considerable amount of time lost making phone calls. Instead of spending hours on the phone with insurance companies, make best use of your staff’s time by checking to see if you have the integrated eligibility feature in your billing software.
Getting started is as easy as getting set up with a clearinghouse (EZClaim clearinghouse partners). Once you are signed up with a clearinghouse for the electronic claim submission program, they will have an integrated eligibility feature that is integrated into EZClaim. Once you sign up with this feature, you can send a batch request of 50 patients at one time and if needed, send multiple requests in a day. Do this by selecting an active patient list collectively or send them individually in smaller amounts. Either way the time savings will be exponential.
Eligibility response reports often come back within seconds making the process nearly real-time. When a response comes back you have the real-time eligibility information. You will get details on if they are covered or not, their active dates, deductibles, co-insurances, co-pays, and what amounts they are subject to and what will be deducted. With EZClaim eligibility integration built in you save valuable time. To learn more contact EZClaim’s website, email, or call 877.650.0904.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.
Apr 5, 2021 | EZClaim Premier, Features, Medical Billing Software Blog
EZClaim medical billing software has many features built into the program to help you submit clean claims for quick payment and some that can be customized to fit your specific needs. This post will look at the ability to create customized validation rules.
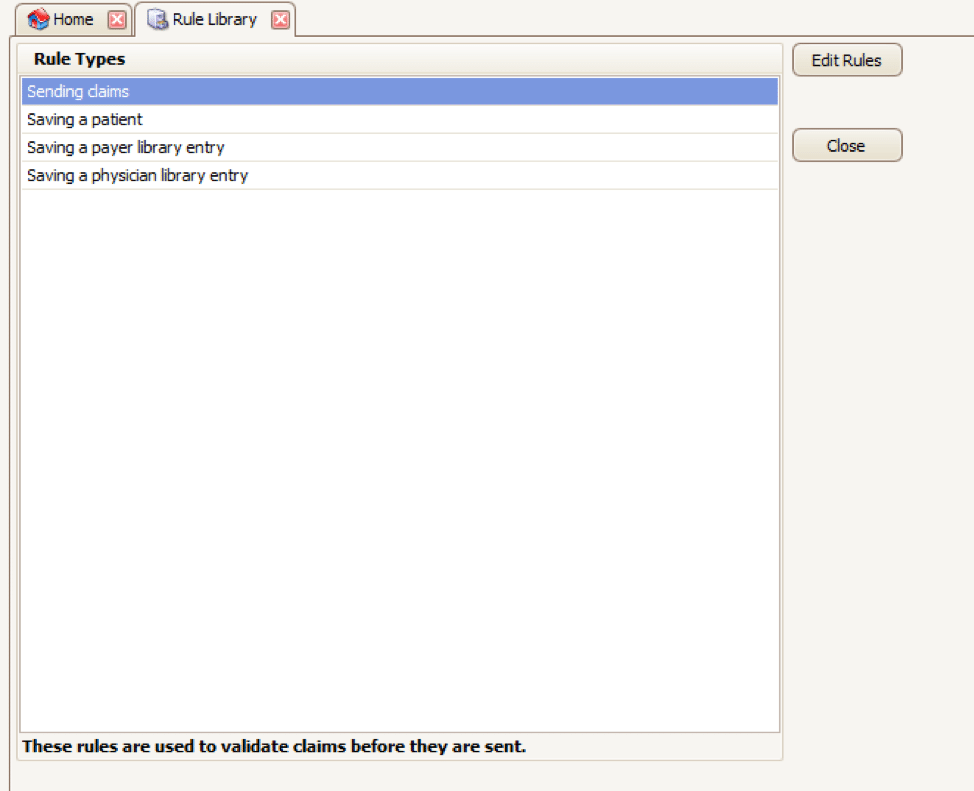
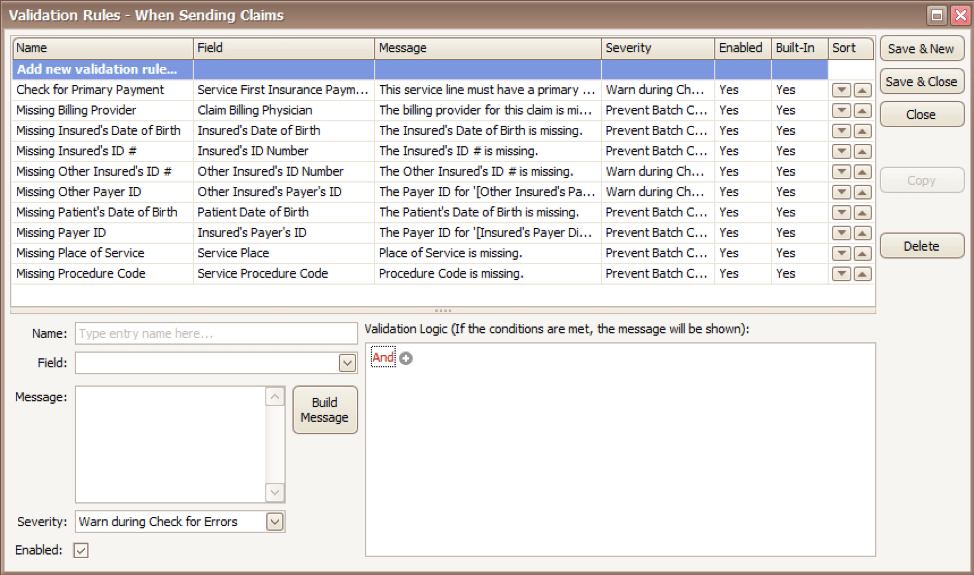
Your EZClaim program already includes standard validation rules. To access these rules and create your own, press CTRL-ALT-V. This will open the Rule Library.
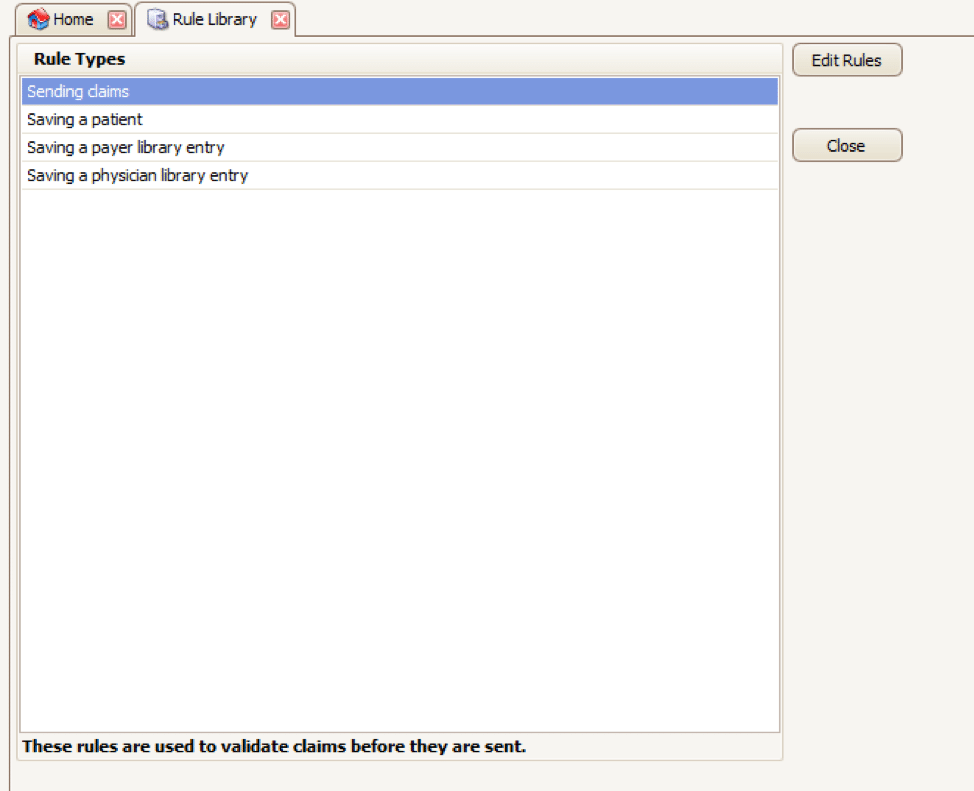
Here you will find four different types of rules to work with, rules related to:
- Sending claims
- Saving a patient
- Saving a payer library entry
- Saving a physician library entry
Now, click on the rule type you would like to work with and click Edit Rules. A list of rules that are already in the program will appear, along with the option at the top to “Add new validation rule“.
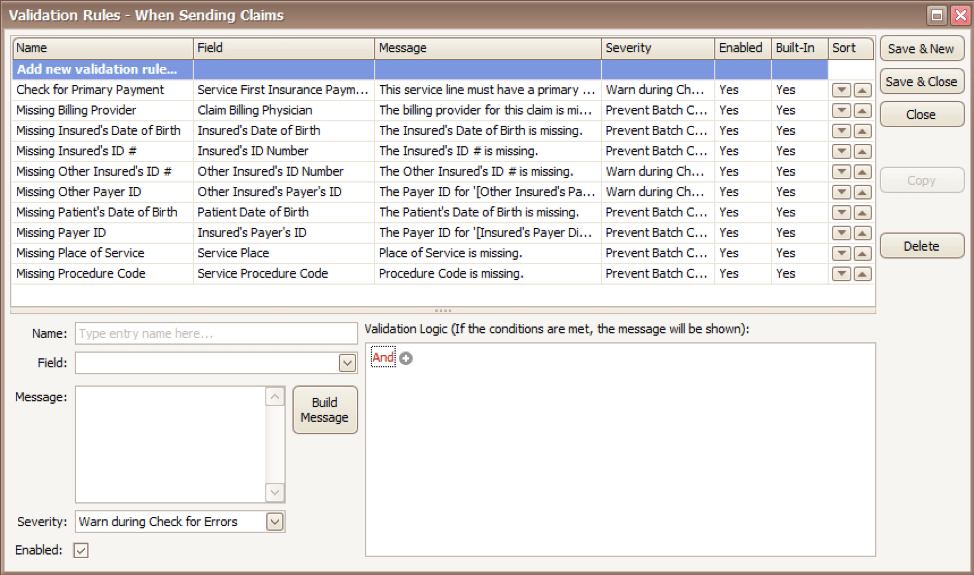
To get started, you will fill in the fields on the bottom left side of the screen:
Name: Name the rule anything you would like
Field: This is the field in Premier that you want to validate
Message: This is the message that will show when the error is encountered (consider using casual wording or extra punctuation so it is easily identified as a custom rule rather than a default rule)
Severity: Do you want the program to simply warn you that there may be an error or stop you from completing the task?
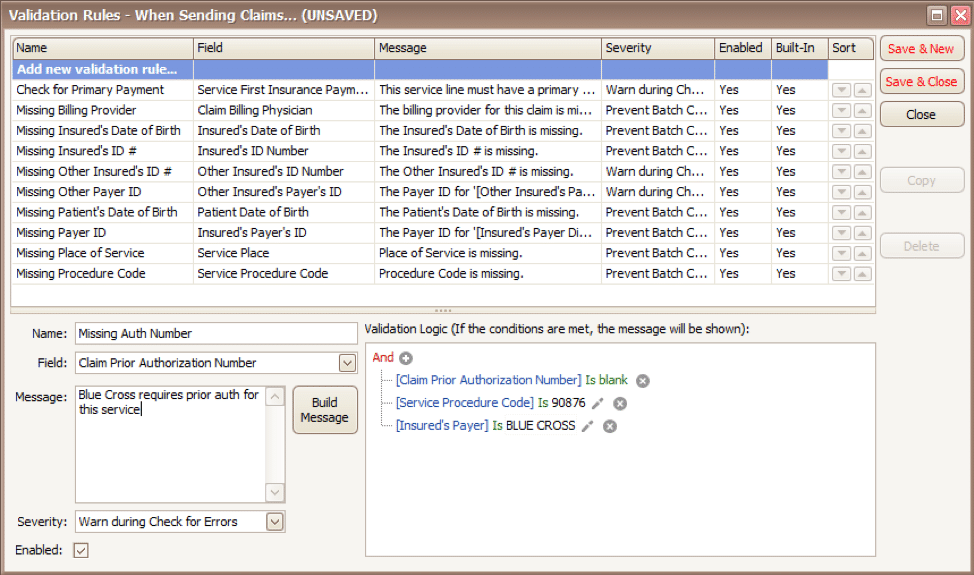
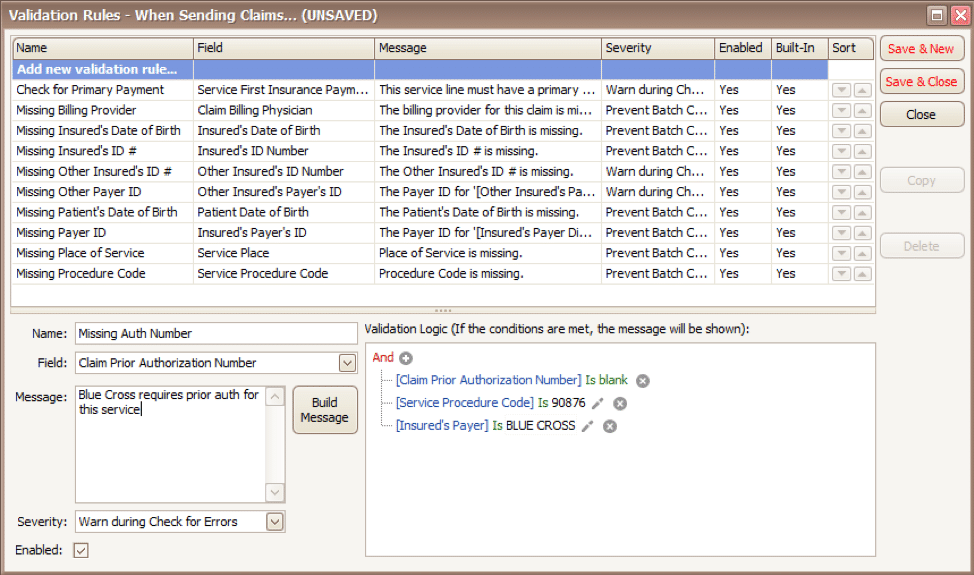
Next, you will build the logic for the validation of the field you have named above. In the example below, the rule has been created to warn users if ALL the following statements are true:
- Authorization Number is blank
- Procedure Code is 90876
- Payer is Blue Cross
Before you begin working with your validation rules it is extremely important to keep the following in mind:
- Rules are created to check for bad or missing data, not to confirm good data.
- Rules in the Sending Claims area may prevent batches from being created.
- If you wish to bypass a built-in validation rule you may disable it, if you want to customize it you can Copy the rule, update, and disable the original rule.
- Rules are the sole responsibility of the practice, EZClaim cannot troubleshoot custom validation rules.
As you can see, custom rules allow you to be very specific and can include multiple data points. Learning to use validation rules can be tricky and may take a few tries to get the rule built correctly. However, once you have the rule in place you can avoid payment delays and needing to resubmit claims.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.