May 29, 2024 | EZClaim, Features
For medical practices of all sizes, the ability to manage patient billing and collections effectively is not just about financial health; it’s a cornerstone of a physician’s capacity to provide ongoing patient care. However, medical billing is often timely and resource-heavy, from the need to file multiple claims, to addressing coding errors, to ensuring the accuracy of technology. Every practice deserves to reap the benefits of a streamlined patient collection process.
Let’s dive into four strategies for streamlining patient collections in medical billing.
Key Strategies for Enhancing Patient Collections
1. Proactive Patient Engagement
Early in the billing cycle, clear communication with patients, including education on accepted payment methods and creating easy-to-understand policies, boosts patient collections across practices of all sizes. How can you expect your patients to pay on time if they aren’t clear on how to pay, or what the process looks like?
Using tools like automated payment reminders and SMS text messages not only adds a personal touch to your practice’s communications but also ensures patients have the information they need to make timely payments.
2. Offering Flexible Payment Options
Making it easy for patients to pay is as important as issuing the patient bill. That’s where flexible payment options come into play, acting as a bridge between the healthcare providers and their patients’ financial realities. A study by Flywire found a whopping 63.4% of patients said they would prefer to pay their medical bills online, compared to 22.5% preferring to pay by check in the mail. 7.3% preferring to pay by phone, and 6.8% preferring to pay in person. This also helps instill patient confidence in the billing process, increasing the likelihood that bills are paid on time and patients avoid medical debt.
Incorporating a mix of payment methods ensures that every patient finds a convenient way to pay their bills. Using a payment processing tool like EZClaimPay can play an instrumental role in improving your practice’s collections by making online payments simple. Integrated tools like EZClaim’s BillFlash electronic statements make it easy for practices to offer online, e-Pay, and even mail-in payments to patients. Send and manage patient billing statements from one centralized location that protects patient data. By enabling your patients to pay online, your practice simplifies the payment process and gives itself the best chance to get paid promptly.
But, it’s not just about the method; it’s also about the plan. Payment plans have shown their worth by allowing patients to manage larger medical expenses over time, making payments more manageable and less intimidating. It’s about giving control back to the patients, allowing them to engage with their healthcare provider on terms that fit their budget.
According to RevSpring, “Among patients who make recurring medical payments, 71.5 percent use ACH, 18.2 percent use credit cards, and 10.2 percent use debit or prepaid debit cards.” The preference for payment convenience and remote bill payment is evident. By facilitating recurring billing, practices not only enhance the chances of receiving payments on time but also simplify their record-keeping, ensuring accurate and reliable patient collections.
3. Transparent Communication
Ensuring transparency and understanding is crucial for enhancing patient collections in medical billing. Here are some ways your practice can foster better communication with patients:
- Be Upfront About Costs: Always inform patients about expected costs before services are rendered to prevent surprises.
- Simplify Payment Policies: Use clear, simple language when explaining payment policies. Avoid complex jargon that might confuse patients.
- Empathetic Financial Discussions: Approach conversations about financial responsibilities with empathy and understanding:
- Acknowledge the stress that medical bills can create.
- Provide clear, patient explanations and be ready to answer questions.
- Offer information about payment plans or assistance programs if necessary.
Communicating with your patients transparently will not only promote on-time payments but also contribute to building a trusting relationship with your patients that emphasizes care over costs.
4. Leverage Automation
Lastly, automation can enhance your practice’s ability to process claims and submit them to payers swiftly, resulting in faster reimbursement. This is crucial for maintaining a healthy cash flow and RCM management as well as getting paid promptly.
Specifically, automation provides healthcare providers with real-time visibility into their revenue cycle, allowing them to track claims at every stage of the billing process. Advanced reporting and analytics make it easy to identify bottlenecks, optimize workflows, and prioritize follow-up with certain patients, ultimately leading to improved cash flow and revenue optimization.
By automating the more troublesome and manual aspects of the billing process, your practice can speed up its operations and move claims through at a considerably faster rate, enhancing the productivity of collections.
Get Started with Simplified Medical Billing
Ready to revolutionize your medical billing process and enhance patient collections? Implementing these key strategies can dramatically improve your practice’s efficiency, patient satisfaction, and financial health. From leveraging cutting-edge payment processing solutions like EZClaimPay to engaging with your patients proactively and offering flexible payment options, we hope we have made the path to a smoother, more efficient collections process clearer.
Don’t let complex billing challenges hold your practice back. Take the first step towards optimized patient collections today—contact us to discover how our solutions can tailor-fit your needs and propel your practice forward.
Learn more about EZClaimPay and how your practice can enhance its collections today!

Jun 29, 2021 | Credit Card Processing, Features, Medical Billing Software Blog
Does your team spend countless hours on the phone attempting to collect payments from patients? Do you know how much of your valuable time is spent performing double data entries of those payments just to keep your books balanced? Do you find yourself wishing you had a one-stop-shop for all your patient payment needs? Well, you are in luck. EZClaimPay has the patient portal feature which allows you and your team to not only save time but makes it easier to collect and record payments.
In 2020, EZClaimPay was launched as a solution to the ever-changing environment of payment reconciliation. This was in response to customers’ difficulties with credit card payment processing. EZClaimPay provides for consolidated reconciliation and a single point of contact for support to make accepting credit and debit card payments painless.
If all that is not enough, the patient portal feature allows for the following:
- Medical staff to text and email patients their statements directly.
- Allows patients to make payments on their mobile devices or online.
- Gives patients the ability to save and print their own receipts.
- Patient payments go directly into your EZClaim account.
- 24-hour a day convenience.
EZClaimPay allows for more freedom to allow patients to pay online, reduced billing errors, increases revenue, and a simplified payment process making the EZClaimPay and the patient portal a no-brainer! For more information contact us or call directly at 877.650.0904.

May 11, 2021 | Features, Medical Billing Software Blog
Can you add up the number of hours your billing team spent during any given week or month waiting on-hold with insurance companies to get patient billing information? Does your staff invest hours of their valuable time seeking out the smallest of details to get paid? Are you aware that integrated eligibility, through EZClaim’s medical billing software, can reduce that time on-hold to a fraction of the total?
It is estimated that the average biller can spend up to 2-hours on-hold just to get an insurance company on the phone. Add to that an average of 10 – 15 minutes to talk through a patient and most companies will only address one or two patients at a time. To add to it often there are multiple insurance companies to call. As you can tell you quickly have a considerable amount of time lost making phone calls. Instead of spending hours on the phone with insurance companies, make best use of your staff’s time by checking to see if you have the integrated eligibility feature in your billing software.
Getting started is as easy as getting set up with a clearinghouse (EZClaim clearinghouse partners). Once you are signed up with a clearinghouse for the electronic claim submission program, they will have an integrated eligibility feature that is integrated into EZClaim. Once you sign up with this feature, you can send a batch request of 50 patients at one time and if needed, send multiple requests in a day. Do this by selecting an active patient list collectively or send them individually in smaller amounts. Either way the time savings will be exponential.
Eligibility response reports often come back within seconds making the process nearly real-time. When a response comes back you have the real-time eligibility information. You will get details on if they are covered or not, their active dates, deductibles, co-insurances, co-pays, and what amounts they are subject to and what will be deducted. With EZClaim eligibility integration built in you save valuable time. To learn more contact EZClaim’s website, email, or call 877.650.0904.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.
Apr 5, 2021 | EZClaim Premier, Features, Medical Billing Software Blog
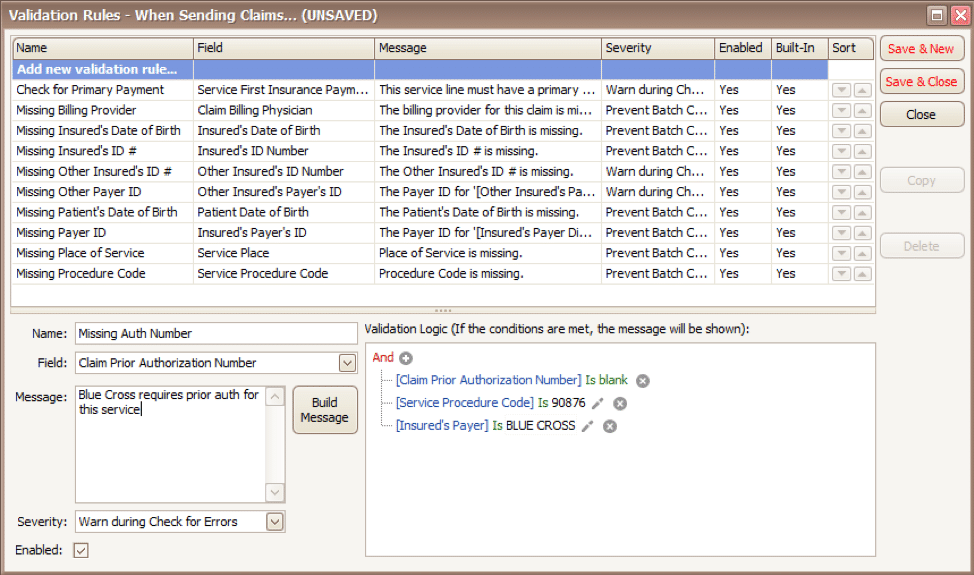
EZClaim medical billing software has many features built into the program to help you submit clean claims for quick payment and some that can be customized to fit your specific needs. This post will look at the ability to create customized validation rules.
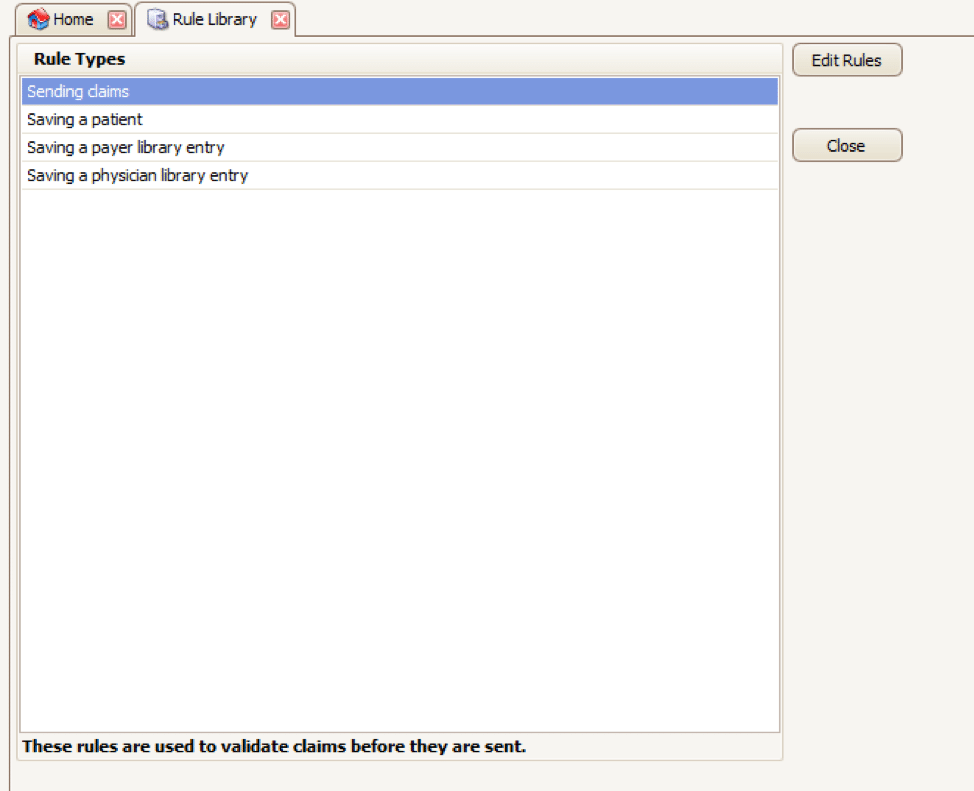
Your EZClaim program already includes standard validation rules. To access these rules and create your own, press CTRL-ALT-V. This will open the Rule Library.
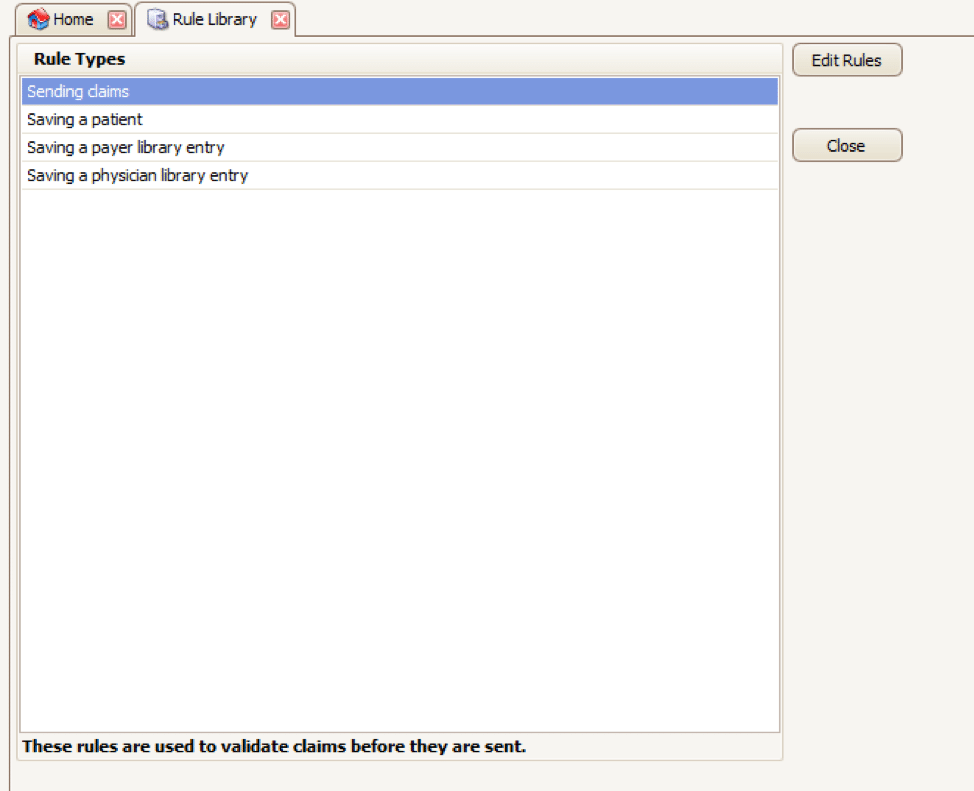
Here you will find four different types of rules to work with, rules related to:
- Sending claims
- Saving a patient
- Saving a payer library entry
- Saving a physician library entry
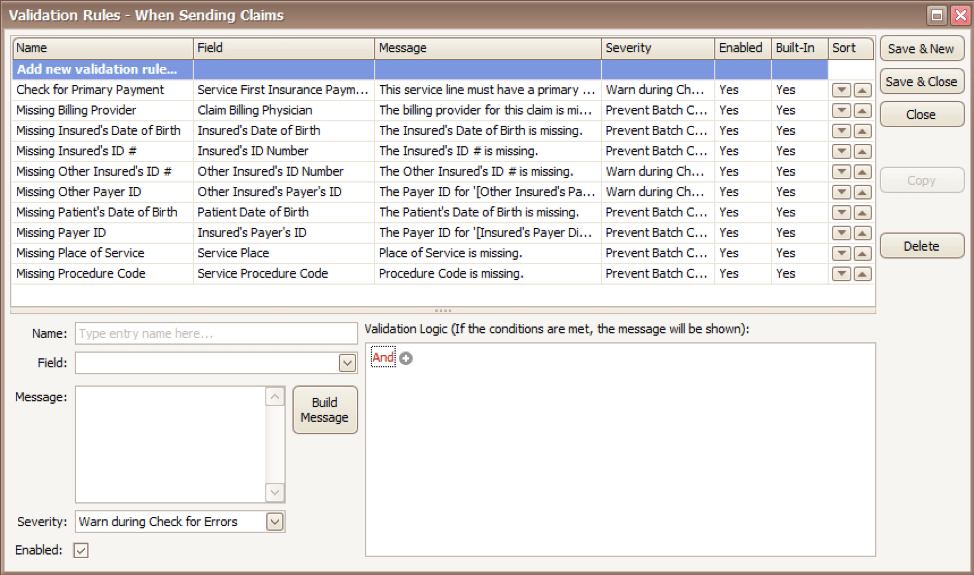
Now, click on the rule type you would like to work with and click Edit Rules. A list of rules that are already in the program will appear, along with the option at the top to “Add new validation rule“.
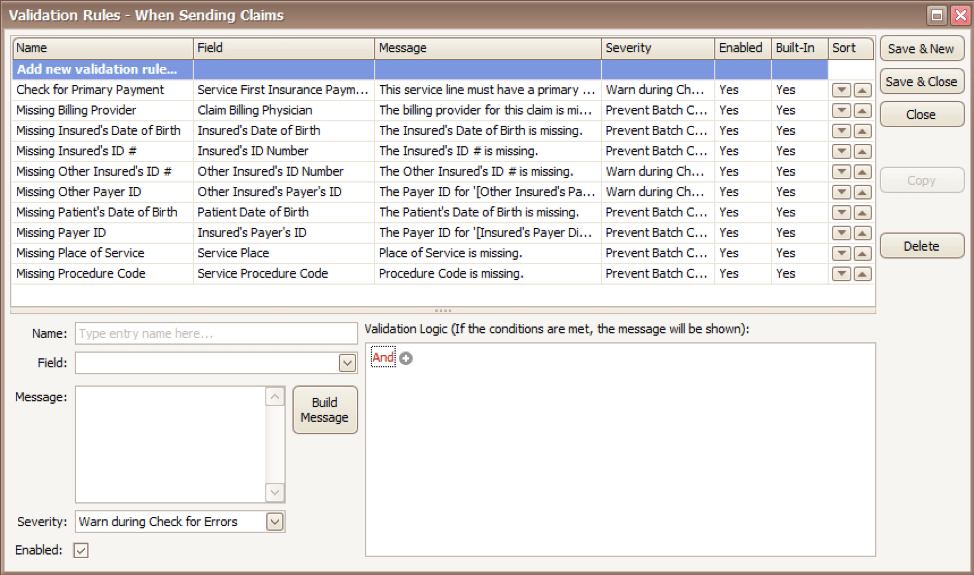
To get started, you will fill in the fields on the bottom left side of the screen:
Name: Name the rule anything you would like
Field: This is the field in Premier that you want to validate
Message: This is the message that will show when the error is encountered (consider using casual wording or extra punctuation so it is easily identified as a custom rule rather than a default rule)
Severity: Do you want the program to simply warn you that there may be an error or stop you from completing the task?
Next, you will build the logic for the validation of the field you have named above. In the example below, the rule has been created to warn users if ALL the following statements are true:
- Authorization Number is blank
- Procedure Code is 90876
- Payer is Blue Cross
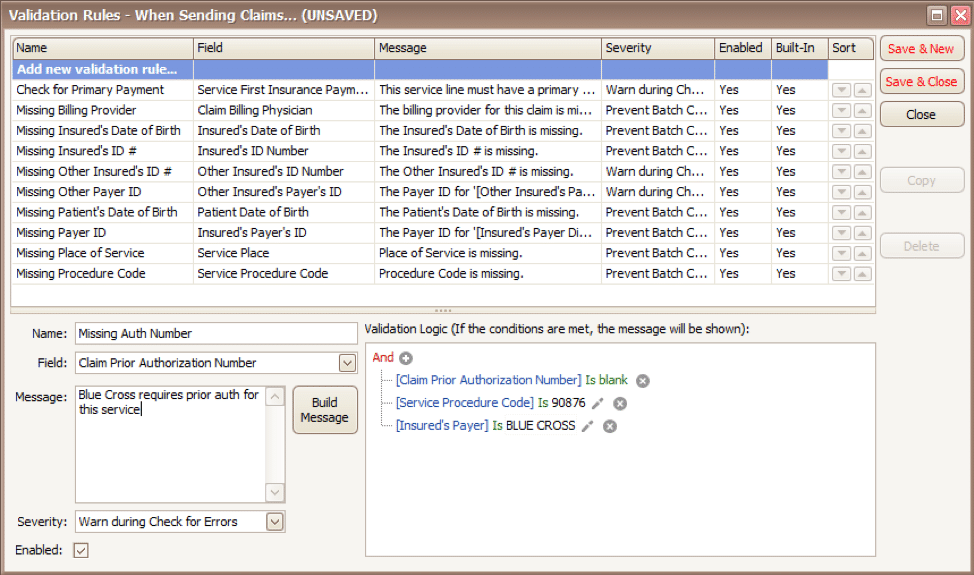
Before you begin working with your validation rules it is extremely important to keep the following in mind:
- Rules are created to check for bad or missing data, not to confirm good data.
- Rules in the Sending Claims area may prevent batches from being created.
- If you wish to bypass a built-in validation rule you may disable it, if you want to customize it you can Copy the rule, update, and disable the original rule.
- Rules are the sole responsibility of the practice, EZClaim cannot troubleshoot custom validation rules.
As you can see, custom rules allow you to be very specific and can include multiple data points. Learning to use validation rules can be tricky and may take a few tries to get the rule built correctly. However, once you have the rule in place you can avoid payment delays and needing to resubmit claims.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.

Feb 9, 2021 | Claims, Electronic Billing, Features, Medical Billing Customer Service, Medical Billing Software Blog
Are you working in the medical billing industry as a biller or an owner of a billing company? If so, the KEY medical billing insights and best practices that came out of our interview with Maura Jansen (VP of Operations) and Jennifer Withington (Director of Revenue) at Missing Piece Billing & Consulting Solutions will be VERY VALUABLE for you to consider.
Jennifer, an expert in understanding the problem-solving techniques and the investigative nature of medical billing, offers insights that both educate and inspire. Maura, an executive member of the billing community, also added an important perspective about EZClaim’s medical billing software. The following are some highlights from our interview.
EZCLAIM: When did you get into the industry?
JENNIFER: “I worked in group homes for the waiver side of group aid and then I went to Missing Piece. Missing Piece primarily deals with ABA providers and provides early intervention rendered to children. For me, the move from waivers with adults to professional billing, indirectly assisting children, was attractive and I took to the billing side of things.”
EZCLAIM: What does that mean when you say you took to the billing side of things?
JENNIFER: “Insurance doesn’t make a lot of sense when you first start. So, I took to the investigative side of making sense of medical billing claims. Figuring out what the payer’s rules are, reading their manuals, and figuring out the technical jargon with the purpose of preventing claim denials was attractive. I liked the puzzle of it.”
EZCLAIM: Are there things that you value in your work that offer meaning to what you do?
JENNIFER: “It’s really when I know that if I do not intercede with the insurance company and get this paid the patient is going to be responsible for the balance. So, to help, I have taken things to the department of insurance, or I have gone ahead and filed that third letter of appeal and really taken the time to research it. Because I don’t want a parent who is already struggling with having a child with more needs than maybe the other children would have, I don’t want them struggling with a $25,000 bill. ABA is extremely expensive because it works. And so, if insurance doesn’t pay it then the only other funder is the parent. And my goal is that parents should not have to pay any more than they absolutely have to.”
EZCLAIM: What are some of the strengths that make you good at what you do?
JENNIFER: “I am a good problem solver. I am good at taking a large problem and breaking it into smaller problems and knocking each one down until I solve the bigger issue. At the end of the day, that’s really what accounts receivable is.”
EZCLAIM: What would be an example of your problem solving on a day-to-day basis?
JENNIFER: “So you always start with the denial and then you have to work back to the billing. For example, if I have a claim denied for services rendered from an out-of-network service provider, but we know we are in-network then my first problem is, are we actually in-network? Then, you go onto the next link which is did the payer recognize you as in-network? It becomes like a decision tree, if you get a ‘yes’ then you are probably done, and you get the claim processed. If it is ‘no’, then you have to start digging with the payers contacting reps, make calls, and supply them with documents to get down to why they don’t have your provider listed within the network. Once you solve that problem, then the claim should be able to be processed. It is either going to pay or deny. Then depending on which one it is, you apply the same technique.”
EZCLAIM: What would you offer someone who is considering entering the field?
JENNIFER: “You should be good at processing and reading information because to get a claim paid you to have to know the rules of engagement. You need to be familiar with how to read a contract, how to read technical information about billing, and have to have a glossary of information about what you are billing. Those are the building blocks to get to know what you are doing.”
EZCLAIM: You work with EZClaim’s medical billing software platform, what role does their software providers and how does that impact your work?
JENNIFER: “EZClaim really serves to eliminate these denials before they happen, which is the ultimate goal of any accounts receivable or billing. EZClaim has edits that we use. It alerts us if the system thinks the claim is a duplicate, for example. It also helps in the set-up of the claim. We load all the fee schedules in EZClaim’s procedure code library and that lets us monitor the charge rate, make sure all the points of billing are on the claim (i.e. correct code, modifier, and charge). They also make sure that the authorization is appended to the claim. And then after we have actually done the work of getting a claim in the system, we use EZClaim reports to audit our own billing. So, we use the EZClaim service report. It makes it easier for us and our providers to see what has been billed and make sure that the billing is correct.”
EZCLAIM: If you were going to share something with your colleagues in the field, what would you share about the software that makes your life easier?
JENNIFER: “Number one, it is not the software itself, it’s the EZClaim staff. Their customer service is far beyond what a normal billing software company provides. If I have a problem, or if I have a report, or if I have a data point that isn’t in any report, they are available and they are there for me. And if they don’t have a solution for the problem, they will provide me with a workaround. So, that is very valuable. That is why Missing Piece works so well with EZClaim because customer service is number one for us, too. They don’t just want to answer your question, they want to help you understand your question.”
“The other thing that I find valuable is that their reporting modules are just a lot more robust than the other billing software companies that I have dealt with.”
EZCLAIM: Maura, do you have any thoughts from an administrative level that you can offer on EZClaim?
MAURA: “Well, when we hire a new person we know that, even if this person has very little experience in the healthcare field, it’s going to be a quick and easy process for them to learn EZClaim… EZClaim has also made it kind of a joy to work with. We really value them as a partner. We love the service they provide, and we value them as a platform.”
ABOUT EZCLAIM:
EZClaim can also help you with medical billing insights since it is a medical billing and scheduling software company. It provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.

Oct 12, 2020 | Electronic Billing, Features, Medical Billing Software Blog
EZClaim Launches EZClaimPay, a new feature in its medical billing software that makes credit card processing painless!
EZClaim, a company with the mission of elevating its clients to stay in front of the ever-changing landscape of medical billing, announced today the launch of its credit card processing feature and service called, EZClaimPay.
EZClaim released the product in August 2020 as a solution to the ever-changing landscape of payment reconciliation. It was cited by customers as a timely response to a ‘pain point’—credit card payment processing—another example of EZClaim’s devotion to their mission.
Dan Loch, VP of Marketing commented that “EZClaim’s goal continues to be making life easier for medical billers at practices and billing firms. EZClaimPay is just one more feature within our mission of living up to that goal.” This feature will help companies get in front of the changes in medical transparency that are coming soon.
EZClaimPay provides for consolidated reconciliation (Payment reports; Chargeback management; and Reconciliation reports) and a single point of contact for support (Hardware; Software; and Payments).
EZClaim has developed a robust payments platform—tightly integrated with their software and support—to make accepting credit cards for payment PAINLESS! EZClaimPay makes software and payments better together.
For more details about EZClaimPay, view this web page: https://ezclaim.com/ezclaimpay/
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides best-in-class customer service and support. To learn more, e-mail them at sales@ezclaim.com or call a representative today at 877.650.0904.