May 12, 2020 | Electronic Billing, EZClaim Premier, Features
A recent medical billing webinar on Telehealth that EZclaim hosted is now available to review.
On April 30th, EZClaim hosted a Telehealth Updates Webinar for our clients with guest speaker Sandy Giangreco Brown – Director of Coding and Revenue Integrity Health Care at CliftonLarsonAllen, LLP
We had one of the largest viewing audiences 101 active attendees in the session. Sandy shared informative billing codes and direct links to update hands-on information for billers actively coding Telehealth sessions. For those of you who missed it, we have provided on our website the recorded session ezclaim.com/webinars and can provide the presentation slides too! Just send a request to sales@ezclaim.com
We continue to get views of this presentation and look forward to hosting more hot topics with the CLA Team.
With the onset of COVID-19 came a great opportunity for clinics and hospitals to offer Telehealth and Communication Technology Based (CTSB) services. The Centers of Medicare and Medicaid Services, or CMS, have provided many updates to the available services that can be provided and billed to the patients to help practices not only stay afloat financially but also and most importantly, to keep their staff safe and provide excellent care to their patients!
There were new guidelines released even after this webinar on 4/30/2020 (which can be found here – https://www.cms.gov/files/document/se20016.pdf, and now includes audio-only Telehealth for services such as psychotherapy, tobacco cessation and medical nutrition counseling as well as diabetes self-management training. CMS is also increasing the payments for the Audio Only services from $14-$41 nationally to $46-$110.
As of April 30, 2020, in order to bill Telehealth, RHCs are now required to bill the G2025–CG–95 from January 27, 2020, to June 30, 2020. Then from July 1, 2020, to the end of the PHE, they will be billing the G2025 with an optional 95 modifier, per CMS SE20016 Medicare Learning Network Transmittal.
FQHCs will need to report three (3) codes for their Telehealth Services:
- G0467 (or other appropriate FQHC specific payment code)
- 99214–95 (or other FQHC PPS Qualifying Payment Code)
- G2025–95
CLA is on the frontlines and closely monitoring and analyzing activities related to Telehealth and other virtual health regulations
CMS Telehealth fact sheet, Frequently Ask Questions:
As your practice adjusts to Telehealth going forward, EZclaim’s medical billing solution can help you simplify patient billing and help you get paid for Telehealth visits. (Our recent medical billing webinar on Telehealth may just help you better understand the current situation).
So, to help you investigate how EZclaim’s medical billing solution may work for you, either schedule a one-on-one consultation with our sales team or download a FREE TRIAL to check out the software yourself. For additional information right now, contact EZclaim’s sales team at 877.650.0904 or send an e-mail to sales@ezclaim.com.
[Contributed by Sandy Giangreco Brown – Director of Coding and Revenue Integrity Health Care, CliftonLarsenAllen LLP]
May 12, 2020 | BillFlash, Features, Medical Billing Software Blog
Telemedicine was already growing in popularity prior to the onset of the Coronavirus pandemic. So, as the adoption rate increases, EZClaim clients may have questions about sending telemedicine charges and getting paid for Telehealth visits.
Telehealth challenges can range from issues with technology to getting paid. With Telehealth becoming the norm for many doctor-patient visits, it is important to have a thoughtful approach in place regarding collecting patient payments. To stay in business, you have to get paid for the work you are doing. So, establishing a process for Telehealth consultations is vital to your business, and it should be a top priority to build a successful program from beginning to end.
The answers to the following questions will help set the baseline for how to collect patient payments for
Telehealth visits:
- What is my process for charging for copays?
- How and when do I collect outstanding balances?
For example, if you collect payment before an in-person visit, you should collect payment before a Telehealth visit, too. There is no need to re-create your process completely. Just change what is needed to match your current in-office routine.
Sending Charges Before a Telehealth Visit
A simple way to send pre-visit charges to patients is to provide them with a link that takes them directly to the payment site. EZClaim’s medical billing solution is integrated with BillFlash LinkPay, which enables customers to provide payment for the upcoming visit. So, before the Telehealth session begins, the practice simply sends a link to their patient via an e-mail or text, making the appointment confirmation and the payment processing part of the check-in process. After the payment transaction is complete, it will immediately show up on the practice’s BillFlash report. LinkPay is designed to be easy to use and doesn’t require patients to remember a login or a chart number.
Here’s how EZClaim enables the process through BillFlash:
- Prior to Telehealth visit, the patient is sent a link to pay through LinkPay, and another link to join the Telehealth call
- The patient pays the required amount through LinkPay, which is immediately confirmed and processed
- The patient joins the Telehealth session
- Results and follow-up are completed electronically
- Insurance billing is completed
- The patient receives a paper statement or eBill notification for any remaining balance
- The patient is directed to pay the remaining balance online at MyProviderLink.com
Automate What Can Be Automated
With so many changes taking place in healthcare, a great way to help protect the financial stability of your practice is to automate what can be automated. This saves your staff time and decreases your cost of doing business.
One way to do this is to set up automatic payment plans for patients, particularly for those who have been hit hard by the economic impact of COVID-19. A payment plan is a good way of keeping the revenue flowing in, and it shows your patients that you are compassionate and willing to help them through these unprecedented times.
BillFlash also securely stores payment information, so patients will not need to re-enter their information every time they pay a new bill.
As you continue to adjust to Telehealth going forward, BillFlash can simplify patient billing and payments significantly and help getting paid for Telehealth visits.
So, for a LIMITED TIME (during May 2020), EZClaim customers can try BillFlash statement and eBill services for FREE for 30 days. Click on this link for more details about BillFlash or try it out for the next month.
For additional information, call BillFlash at 435-940-9123, or contact EZclaim’s support team at 877.650.0904 or support@ezclaim.com.
[Contributed by James Easley VP, Marketing NexTrust Inc.]

May 12, 2020 | Live Compliance
Ransomware Targeting Medical Billing Companies
As the number of healthcare providers taking advantage of Telehealth increases during this uncertain time, the number of ransomware attacks continues to increase as well.
Ransomware is a type of malicious software designed to block access to a computer system until a sum of money is paid. Microsoft says, “Multiple ransomware groups that have been accumulating access and maintaining persistence on target networks for several months activated dozens of ransomware deployments in the first two weeks of April 2020.”
The attacks are targeted towards aid organizations, medical billing companies, manufacturing, transport, government institutions, and educational software providers, however, Microsoft says that it doesn’t stop with critical service groups and suggests all networks are aware of these attacks and taking necessary steps to limit risk. NetWalker ransomware, for example, gained notoriety for targeting hospitals and healthcare providers with e-mails claiming to provide information about COVID-19.
Have you had an Accurate and Thorough Security Risk Assessment and/or penetration testing?
If you haven’t completed an accurate and thorough security risk assessment, you could also be penalized under ‘willful neglect’ (this category alone is $50,000 per violation!) in addition to the higher risk of ransomware attacks. What we do is keep this from ever being a worry for you! We perform your security risk assessment and manage all of your requirements, in a clean, organized cloud-based portal.
Don’t risk your company’s future, especially when we are offering a FREE Organization Assessment to help determine your company’s status.
It’s easy! Call us at (980) 999-1585, or email me, Jim Johnson at jim@LiveCompliance.com or visit
www.LiveCompliance.com
Live Compliance has partnered with EZClaim medical billing software to strengthen what they can provide for you. It provides all of your HIPAA Privacy, Security Requirements, and Measures. HIPAA compliance is a requirement for Covered Entities and Business Associates to safeguard personal, private, and protected health information—allowing organizations to relinquish the struggle of compliance requirements.
You can investigate the EZClaim medical billing software by either downloading a FREE DEMO or just contact our knowledgeable sales staff to answer any and all of your questions by phone at (877) 650-0904 or by e-mail at support@ezclaim.com.
[ Contributed by Jim Johnson of Live Compliance ]

Apr 13, 2020 | Medical Billing Software Blog, Revenue, Trizetto Partner Solutions
Because of COVID-19, some practices are doing triage from the car before they will allow a patient into their offices. Practices should also take a ‘cue’ from this by instituting protective measures for their finances.
I went to the doctor for a regular visit last week, which seemed anything but regular. I sat in the car and called to let them know I had arrived. They verified my demographics and insurance information over the phone; me in the parking lot, them in the office. The MA came out with her PPE and took my temperature, found me to be fever free so I could enter the building.
My nurse practitioner came in for our visit. We went about our appointment as usual except this time she took my superbill upfront herself and handed it to the check-out staff member. We scheduled a Telehealth visit instead of a traditional office visit. At the checkout desk, I said “I’m pretty sure I have a balance from the last visit, can I take care of that today?”. I loved where their heart is at, but I was sad to hear her say “You do, but we aren’t worried about that today. Just pay when you get the next statement.”
With so many things in chaos right now, so much thrown at you, and out of your control – let us not forget about the protective measures you can put in place for your practice. This is the time to get some vitals and triage from the car, before blindly allowing the chaos into your business. So, what should you be tracking?
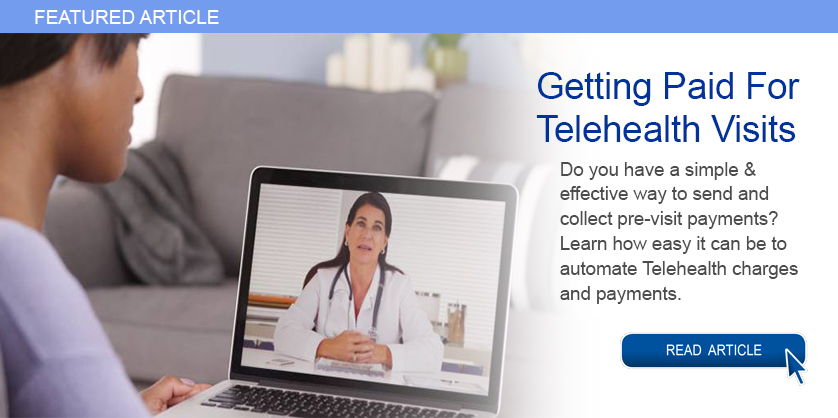
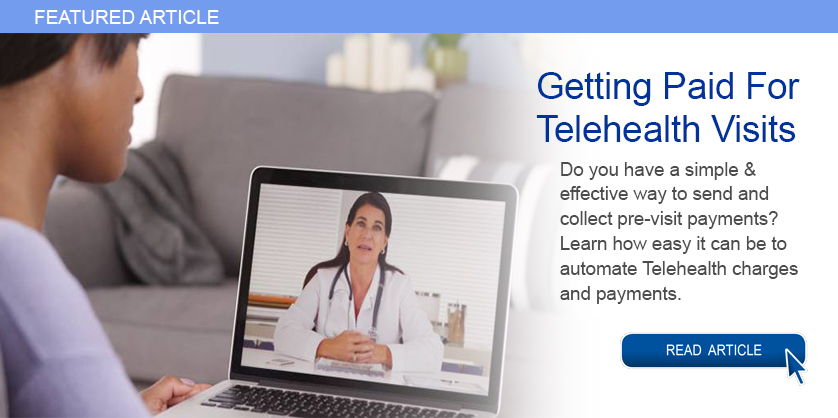
Start with basics – look at the aging balances. More than likely, you have money on the table! In EZClaim, you have the option to run full aging, but the more efficient option is running the Insurance Follow Up report and the Patient Follow Up report. Just running these reports will let you know where there is money that needs to be collected. In addition – it just may show you that it is time to reevaluate policies and procedures in your office related to patient balances and insurance follow-up. Here is a peek at what these two reports can do for you.
Patient Follow Up Report: This report will show you balances that are outstanding with your patients. While this may not be the easiest time to ask patients to pay their balances, there are steps you want to consider:
- Consider what you will do with lingering patient balances. The Patient Follow Up report will show how many statements have been sent since the last patient payment. If you have sent several statements is it worth continued efforts?
- Contact your patients to see if they can pay with an HSA or FSA account
- Offer to set up a payment plan
- Write off the balance as a bad debt or a one-time professional courtesy
- Consider sending the account to collections
- Use technology to your advantage. Take this time to consider enabling online payment options.
- Create or revise patient payment policies and train your staff on these policies
Insurance Follow Up Report: This report will show your balances that are outstanding with insurance companies. Some of the useful features of this report include:
- Ability to see the aged balances by the payer. This lets you get the biggest bang for your buck. Look for payers that have a large percentage of balances in the oldest buckets and work those first.
- All the information you need for calling the insurance is right there on the report. You will have easy access to the date of birth, member ID number, and claim totals on the report.
- During your research, you will find common themes. Use these themes to update your office procedures and train your staff to eliminate errors so that claims get paid quicker.
EZclaim billing software can help you manage your office’s finances. Visit our website to find out more about our solutions: https://ezclaim.com/
[ Contribution by Stephanie Cremeans with EZClaim ]
Mar 23, 2020 | Uncategorized
During these unprecedented times, EZclaim is monitoring Coronavirus (COVID-19) developments, and are working to maintain the safety of our customers and employees. We are doing this by following the guidelines set forth by our state and local governments, and the recommendations from the CDC.
To enhance the safety of our employees, families, and communities, EZClaim is transitioning to a remote workforce to continue to serve our clients during this difficult period. We will remain available and anticipate no disruption to our service or support.
Feel free to e-mail us or visit the contact page on our website to issue any questions or concerns.
Thank you for your patience, and please be safe!
Sincerely,
EZclaim