May 11, 2021 | Features, Medical Billing Software Blog
Can you add up the number of hours your billing team spent during any given week or month waiting on-hold with insurance companies to get patient billing information? Does your staff invest hours of their valuable time seeking out the smallest of details to get paid? Are you aware that integrated eligibility, through EZClaim’s medical billing software, can reduce that time on-hold to a fraction of the total?
It is estimated that the average biller can spend up to 2-hours on-hold just to get an insurance company on the phone. Add to that an average of 10 – 15 minutes to talk through a patient and most companies will only address one or two patients at a time. To add to it often there are multiple insurance companies to call. As you can tell you quickly have a considerable amount of time lost making phone calls. Instead of spending hours on the phone with insurance companies, make best use of your staff’s time by checking to see if you have the integrated eligibility feature in your billing software.
Getting started is as easy as getting set up with a clearinghouse (EZClaim clearinghouse partners). Once you are signed up with a clearinghouse for the electronic claim submission program, they will have an integrated eligibility feature that is integrated into EZClaim. Once you sign up with this feature, you can send a batch request of 50 patients at one time and if needed, send multiple requests in a day. Do this by selecting an active patient list collectively or send them individually in smaller amounts. Either way the time savings will be exponential.
Eligibility response reports often come back within seconds making the process nearly real-time. When a response comes back you have the real-time eligibility information. You will get details on if they are covered or not, their active dates, deductibles, co-insurances, co-pays, and what amounts they are subject to and what will be deducted. With EZClaim eligibility integration built in you save valuable time. To learn more contact EZClaim’s website, email, or call 877.650.0904.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.

Mar 10, 2021 | Credit Card Processing, Medical Billing Customer Service, Medical Billing Software Blog, Trizetto Partner Solutions
What is Price Transparency?
It’s a story we hear too often. A person visits a hospital for a medical issue—whether it be a trip to the emergency room for a broken arm or a pre-scheduled appointment for a headache that just won’t go away—and receives a myriad of services and tests. Then comes the dreaded bill in the mail a few weeks later. Although they may inquire about an estimate at the time of service or have an idea of their coverage, the exact financial responsibility is often a mystery until that bill arrives. While the changes vary greatly, one thing that is certain: many people have trouble with their out-of-pocket costs. So much so that a recent survey from The Commonwealth Fund found that 72 million Americans have some sort of trouble with medical debt.
So, on January 1, 2021, the price transparency rule was put into effect—from the Centers for Medicare and Medicaid Services (CMS)—requiring all hospitals within the United States hospitals to publish the prices of various medical procedures. In particular, standard charges for services and items must be published online, available for patients to access. Until now, these prices were hard to find. The timing of this change—the beginning of the calendar year—comes at a time when healthcare pricing is top of mind since many customers most likely renewed or changed insurance carriers and coverage on January 1, 2021. With this comes a focus on out-of-pocket costs, deductibles, and more.
What Brought About This Radical Change?
Part of this change can be attributed to the consumers themselves. With the increase in high deductible health plans and increased out-of-pocket costs, finances are top of mind. In addition to these factors, today’s consumers demand a better overall patient experience. With the prevalence of online shopping, patients expect the same seamless transaction at the hospital that they receive with companies like Amazon, Walmart, and Home Depot. Just as consumers read product reviews before placing an item in their online shopping cart, patients research services and access peer reviews of physicians before they go to the office. In short, they want to be knowledgeable about their healthcare and crave tailored services with exceptional customer service.
Many believe this change will be well received, with Forbes calling the ruling a “gift to all Americans.” From the consumer’s standpoint, it will now be easier to make educated decisions based on cost. This will then cut down on the “unknown”—hopefully eliminating those hefty surprise bills—and opens the door to comparison shopping. Advocates are hoping this newfound transparency will eventually lower costs, with the competition eventually driving down the prices.
How Can Healthcare Organizations Navigate This Change?
This will not only promote transparency but will also increase convenience. By enabling patients to access and pay their bills on their own schedule with easy-to-implement solutions, organizations are meeting them halfway, so to speak. With easy-to-understand statements, integrated credit card processing, and 24/7 payment portals, it is no longer a hassle to manage medical financials. For healthcare organizations, facilitating proactive management of a person’s cost of care accelerates revenue collections and patient satisfaction improves.
In the larger sense, executives recognize that patients are taking more stock in their personal care. In order to thrive, hospitals and health systems must work toward creating the optimal patient experience, beyond just price transparency. With this, providers should aim to be more engaged and C-suite executives should try to provide additional benefits to their patients.
What Will This Mean for the Future of the Industry?
Only time will tell what the price transparency will mean for the industry. However, it is safe to say that this concept has the possibility to shape healthcare policies and processes for years to come.
So, for more information on solutions that equip you to have informed conversations about eligibility and financial responsibility, contact one of EZClaim’s partners, TriZetto Provider Solutions, to talk with one of their representatives today.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call them today at 877.650.0904.
[ Article contributed by TriZetto Provider Solutions Editorial Team ]
Mar 10, 2021 | Medical Billing Software Blog, Partner, Waystar
New Patient Survey About Price Transparency Rule
With the cost of insurance premiums and deductibles both on the rise, patients have begun taking on greater responsibility for paying for healthcare than ever before. In return, they are becoming more discerning shoppers and expect more from the patient experience that their providers are delivering. One of the biggest steps that have been taken to create a more standardized, consumer-like experience is the introduction of the final price transparency rule from the Centers for Medicare and Medicaid Services.
More than half of consumers have received an unexpected medical bill
Despite the $3.81 trillion that was spent on healthcare in 2019, America’s healthcare payments system has long remained opaque and broken. Patients are frequently faced with unexpected or surprisingly high medical bills, discover too late that a provider they’d been told was in-network was actually out of network, and are forced to wait 60-90 days to receive their medical bills.
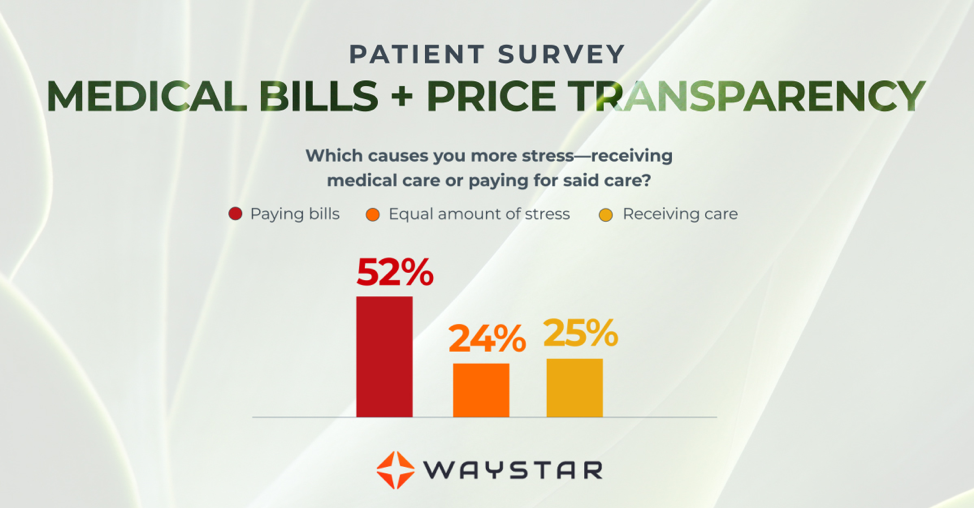
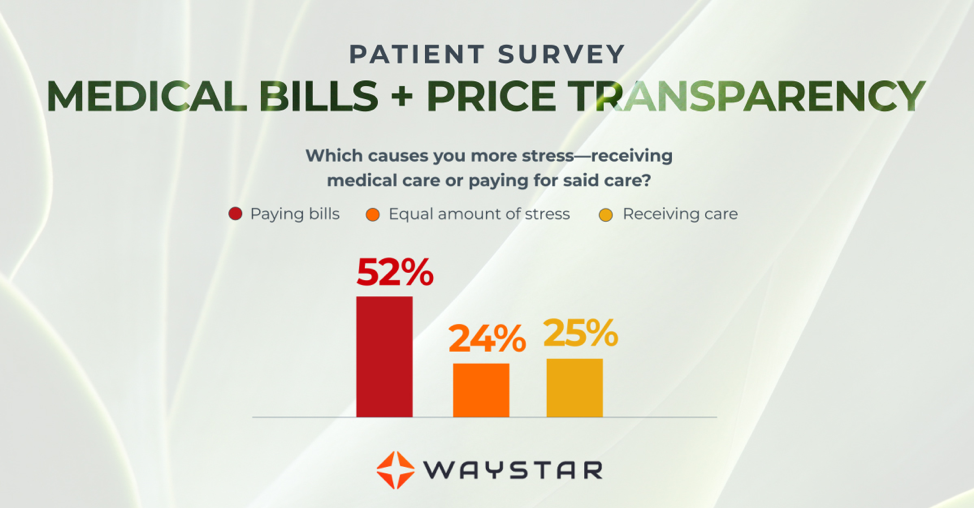
Patients are more concerned about billing than the quality of care
In October 2020, Waystar surveyed 1,000 consumers about their experiences with medical bills, and awareness and attitudes towards the upcoming price transparency rule. More than half of respondents have received an unexpected medical bill, meaning that they assumed a service was covered by insurance and it ultimately was not, or the amount they expected to pay out of pocket was different from the bill they received.
> > > CLICK HERE To Read the Results of the Waystar Survey < < <
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call them today at 877.650.0904.
[ Article contributed by Waystar ]

Oct 12, 2020 | Partner, Trizetto Partner Solutions, Webinar
Reserve your place for a webinar that will inform you on how to increase your revenue with a proper medical billing verification strategy.
With increased patient financial responsibility, it’s extremely important to proactively check your patients’ benefits coverage and provide payment estimates to avoid any unexpected costs. By enhancing your medical billing verification strategy and providing patient financial transparency upfront, it increases the likelihood that you’ll rake in more revenue this season.
Join EZClaim and TriZetto Provider Solutions, a Cognizant Company, for a webinar on Thursday, October 29, 2020 at 1 p.m. ET, to discover strategies your practice can catch falling revenue through seamless integration and automation.
During This Webinar We Will Discuss:
• Patient Responsibility Estimation: Quickly obtain patient financial estimates at the point of service to help increase patient revenue, decrease billing costs, and improve patient satisfaction through price transparency.
• Integrated Eligibility: Connect to payers through a single application to get the most up-to-date information on patient coverage, co-pays, deductibles, and more. Proactively verify patient eligibility, for up to 50 patients at a time directly from your EZClaim Premier program.
• Insurance Eligibility Discovery: Submit a real-time eligibility request using minimal data and identify a patient’s insurance carrier in a matter of seconds. Maintain groups of your common payers and easily locate active patients and full eligibility benefits on our website.
RESERVE YOUR PLACE NOW!
ABOUT THE PRESENTERS:
EZCLAIM: EZClaim is a medical billing and scheduling software company that provides best-in-class customer service and support. To learn more, e-mail them at sales@ezclaim.com or call a representative today at 877.650.0904.
TRIZETTO: TriZetto combines innovative, proven products with an exacting commitment to serving our customers, in order to provide you with the tools you need to effectively manage your reimbursement cycle.