Jul 3, 2022 | Partner, Trizetto Partner Solutions
It’s safe to say that healthcare practitioners are well aware of the importance of credentialing. Beyond the legalities required of practicing physicians, credentials are needed for a practice’s revenue cycle to function properly. If providers aren’t enrolled with payers, they can’t receive payment for submitted claims. It’s as simple as that.
New and existing providers are required to maintain credentials and it’s not an easy process, even for the most well-oiled office. In order to take on the most patients and collect optimal revenue, practices also need to accept a wide array of payers. In fact, there has been a 5 percent uptick in providers enrolled with 10-20 payers, according to VerityStream’s 2018 Provider Enrollment Survey. Gaining enrollment with these payers involves verifying qualifications in order to accept patients, submit claims and ensure a steady stream of cash. Administrators need to collect the educational history of providers, fill out forms and submit the applications. It sounds easy enough, right?
Think again. There are hours of administrative work needed and a high risk for human error, with any hiccup in the process likely causing delays. It’s been said that up to 85% of credentialing applications are incomplete, which could cause delayed billing, lost revenue or even audits.
When it comes to credentialing, time is money. A 2016 survey by Merritt Hawkins found that a non-credentialed doctor was losing approximately $6,600 a day. Multiply that by the total amount of physicians in a given practice, and the potential losses are staggering.
Credentialing is a necessary evil, so do you handle in house or outsource? That’s the million dollar question. Utilizing current staff resources sounds like the easy solution, but does your organization have a dedicated employee to focus on your credentialing needs? Probably not. Chances are, this employee is pulled in many directions and isn’t able to dedicate time solely to credentialing. And if you do plan to handle the process with current staff, are your employees well-versed in all payers and their processes? Factor in learning curves or potential staff turnover and the time associated with training new employees and the not-so obvious financial costs quickly add up.
So how does the average practice streamline the process and ensure that credentials are gained as painlessly as possible? The old adage “you get what you pay for” could easily apply to this scenario. Hiring an outside resource means you are essentially paying for expertise and efficiency, which will save time and money in the long run. Why wouldn’t you want to utilize expert resources with in-depth knowledge of payer and state nuances? However, before making a decision, you need to know how much your practice could save by using a third party. Knowledge is power and having an accurate picture of your potential revenue is the first step to determining the best option for your organization.
Access the credentialing ROI calculator from TriZetto Provider Solutions, a Cognizant Company, to receive an estimate of potential revenue savings. Discover the hidden costs associated with the credentialing process and see just how much revenue your practice could be leaving on the table. You’ll gain enrollments quickly and accurately, keep employee satisfaction levels high (since they won’t be burdened by the process) and ultimately, increase revenue.
Don’t allow the complicated payer credentialing and enrollment process to be a burden on your practice. The credentialing experts at TriZetto Provider Solutions have experience working with various payers and providers of all backgrounds. Our team will collect and submit information in a timely manner and perform all necessary follow-up tasks. Let us lighten your load so you can focus on patient care and growing your practice.
[Contribution by TriZetto Provider Solutions Editorial Team]

Jun 15, 2021 | Claims, Credit Card Processing, Medical Billing Customer Service, Medical Billing Software Blog
Are you or your staff having to enter every patient into your EHR program and then again into EZClaim? There is an easier way! Integrating your programs will put an end to duplicate data entry, saving your practice time and money!
So, what exactly is an interface and how does it work? An interface is a way for two programs to share information. For EZClaim clients, the interface can be set up to share data from your EHR program to EZClaim. Your EHR can give you specifics on how to send the data to EZClaim.
In EZClaim you will have an opportunity to review the file prior to saving the data. When you complete the import process, your claims will be created, and libraries will be updated. In addition to creating your claims for each visit, an interface can also create Physician/Facility library entries, as well as Payer library entries, and create new or update existing patient accounts.
If you are working with one of our partner EHRs (Visit our Partner List) the integration between programs can be set up quickly and easily. Since the process varies slightly depending on the EHR you are using, time to complete the integration request will vary.
If you are not using a partner EHR, you may still be able to integrate with EZClaim.
Following are some options:
- In our Online Help File the format types and specifications are available for you to share with your EHR vendor. If they can provide a file in one of the required formats you will be able to import your data.
- You may consider using a third party to write a custom interface for you. If you would like more information on this, contact EZClaim and we will be happy to provide information on consultants who are familiar with the EZClaim platform.
If you have questions, please submit them via email to support@ezclaim.com so a technician can review them and get back with you.
Apr 5, 2021 | EZClaim Premier, Features, Medical Billing Software Blog
EZClaim medical billing software has many features built into the program to help you submit clean claims for quick payment and some that can be customized to fit your specific needs. This post will look at the ability to create customized validation rules.
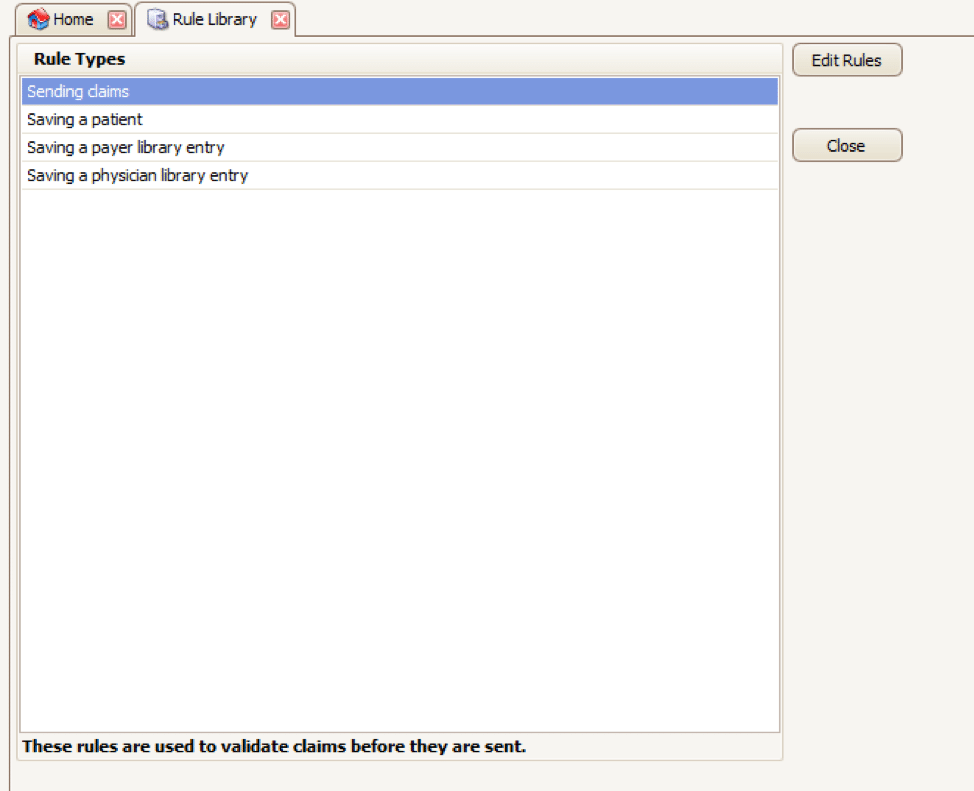
Your EZClaim program already includes standard validation rules. To access these rules and create your own, press CTRL-ALT-V. This will open the Rule Library.
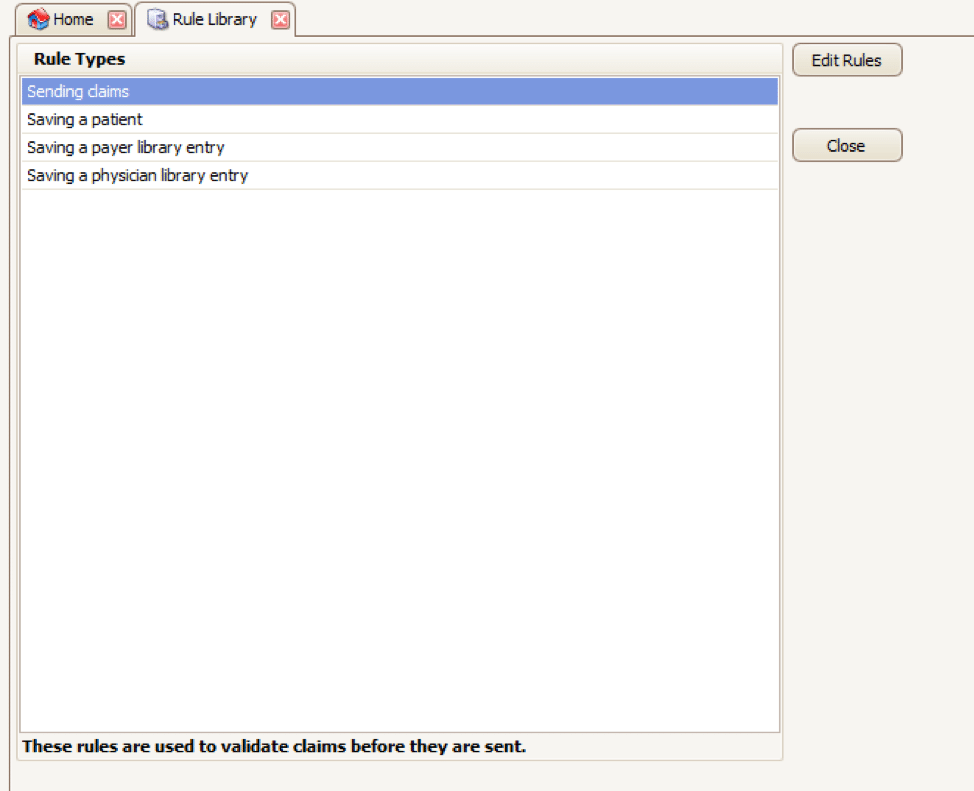
Here you will find four different types of rules to work with, rules related to:
- Sending claims
- Saving a patient
- Saving a payer library entry
- Saving a physician library entry
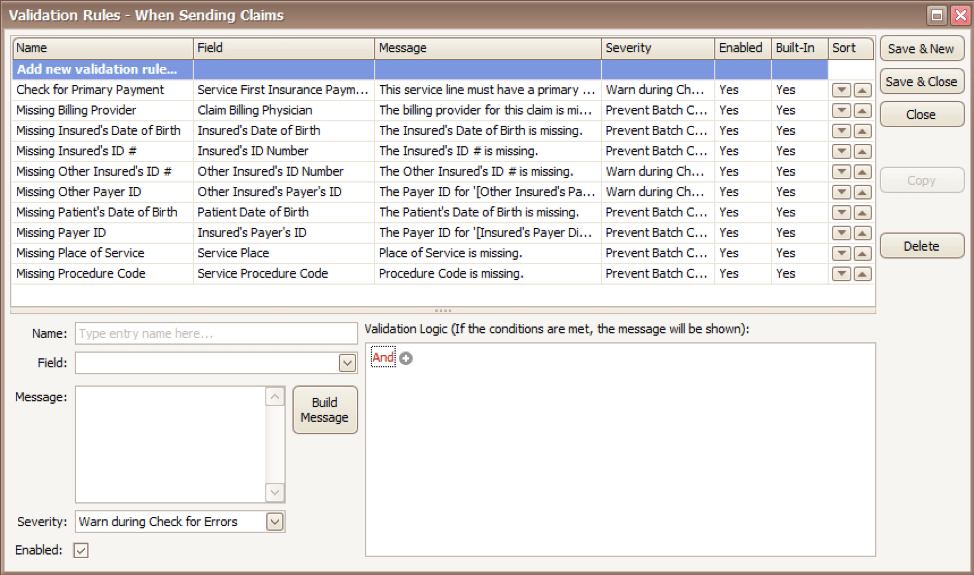
Now, click on the rule type you would like to work with and click Edit Rules. A list of rules that are already in the program will appear, along with the option at the top to “Add new validation rule“.
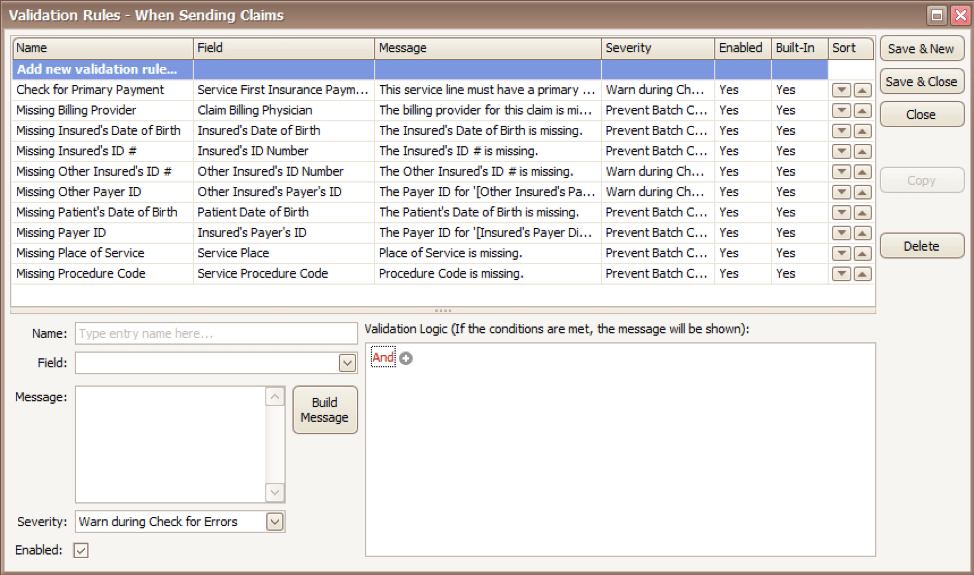
To get started, you will fill in the fields on the bottom left side of the screen:
Name: Name the rule anything you would like
Field: This is the field in Premier that you want to validate
Message: This is the message that will show when the error is encountered (consider using casual wording or extra punctuation so it is easily identified as a custom rule rather than a default rule)
Severity: Do you want the program to simply warn you that there may be an error or stop you from completing the task?
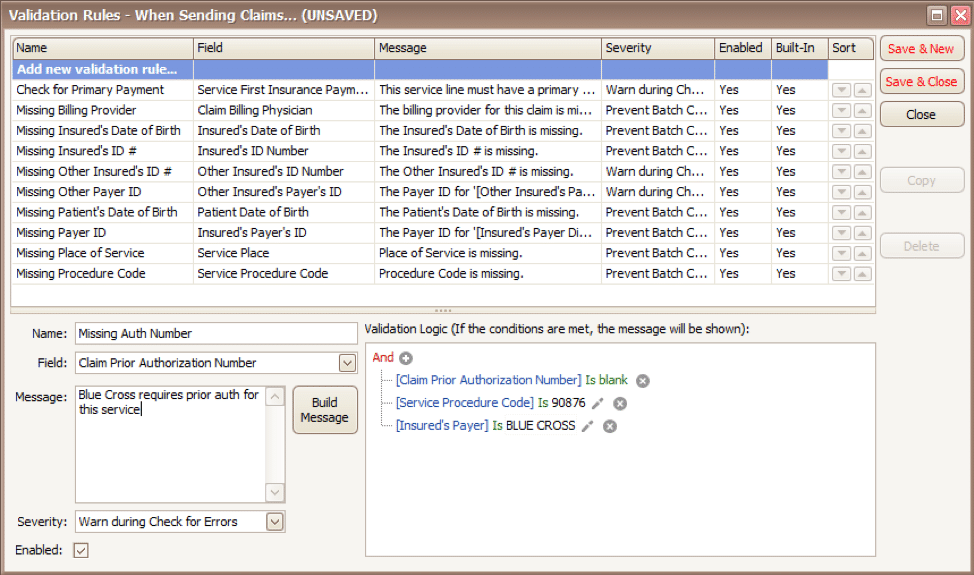
Next, you will build the logic for the validation of the field you have named above. In the example below, the rule has been created to warn users if ALL the following statements are true:
- Authorization Number is blank
- Procedure Code is 90876
- Payer is Blue Cross
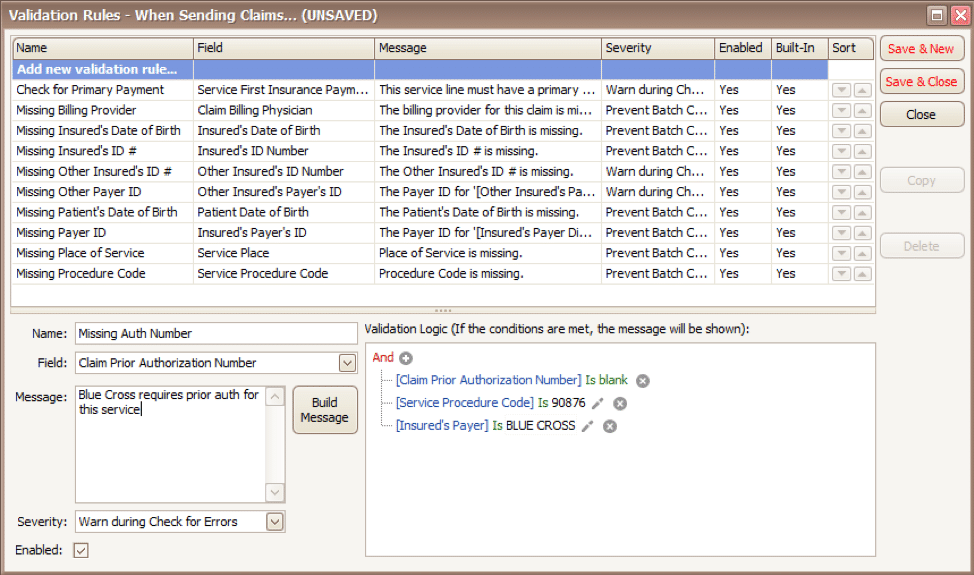
Before you begin working with your validation rules it is extremely important to keep the following in mind:
- Rules are created to check for bad or missing data, not to confirm good data.
- Rules in the Sending Claims area may prevent batches from being created.
- If you wish to bypass a built-in validation rule you may disable it, if you want to customize it you can Copy the rule, update, and disable the original rule.
- Rules are the sole responsibility of the practice, EZClaim cannot troubleshoot custom validation rules.
As you can see, custom rules allow you to be very specific and can include multiple data points. Learning to use validation rules can be tricky and may take a few tries to get the rule built correctly. However, once you have the rule in place you can avoid payment delays and needing to resubmit claims.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.
Mar 10, 2021 | BillFlash, Claims, collections, Credit Card Processing, Fullsteam, Medical Billing Software Blog, Revenue
How to Modernize Your Medical Billing Payments Now
It is now very important to modernize medical billing payments capabilities since upwards of 80% of medical services that don’t get paid by insurance, never get paid!
Are you tired of providing medical services and not getting paid? Have you billed patients for their medical visit or co-pay just to find out that the bill showed up in collections? Are you looking for a better way to use modern technology to increase the number of medical claims being paid on time? If you own a medical practice or work in the medical billing industry, then chances are you have answered each question with a hearty “Yes!”
Last month, medical billing industry leaders came together to discuss how medical practices can streamline their payment systems and integrate credit card processing into their billing system. [ Participants: Dan Loch (VP of Sales & Marketing, EZClaim), Tony Peterson (VP of Business Development, BillFlash), and Michael Jones (Payment Services Analyst, FullSteam) all joined host Susan Martinez (Sales Consultant, EZClaim) ].
[ Click Here to LISTEN to the Exclusive Podcast ]
[ Click Here to VIEW the Exclusive Video ]
KEYS That Came Out of the Discussion:
• CHANGING SYSTEMS AND PROCESSES: The practices that are winning in the payment collections game, and seeing the highest percentage of claims paid, are the offices that have updated their systems from the old school and traditional forms of payment collection to the modern, state-of-the-art systems with payment integration. Plain and simple, this means first educating the patient from the moment they walk in the door and streamlining your payments into one medical billing system to prevent human error. [ Click here to LEARN MORE ].
• STREAMLINING CREDIT CARD PROCESSING: Practices often have jumped headlong into credit card processing by using simple systems with variable fees like Square or Stripe. The problem with that is two-fold: First, understanding processing fees, and secondly, avoiding the errors that occur in the steps of processing those purchases over to the billing record. However, now EZClaim’s medical billing software has an integrated payment feature—which streamlines the billing and simplifies the fees. [ Click here to LEARN MORE ].
These are only a few of the very informational topics that were discussed during this podcast. If you are interested in learning how your practice can put these systems in place, increase patient payments, and simplify your billing process in your office, then click here to listen to the podcast and prepare to learn some new, up-to-the-minute ‘insights’ on modern medical billing systems.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call them today at 877.650.0904.

Feb 9, 2021 | Electronic Billing, Medical Billing Software Blog, Partner
Do you have a fee schedule? If so, do you maintain it on a regular basis?
Well, this is an easy step to skip, but an annual review could put some extra cash in your pocket and help you keep a better handle on how much collectible money you have outstanding. Here are three things you should consider when creating or maintaining your fee schedule:
1. Mark Up the Charge Amount: Did you know that most payers will not pay you more than what you charge, even if you charge less than the allowed amount? They will accept whatever charge amount you have and adjust the difference, but they won’t pay you more than you charge. This can really cost your practice!
2. Allowed Amounts Change: In addition to payers updating the allowed amount for services, many insurances are offering incentive-based programs you may be eligible to collect a percentage over the allowed amount! If you are basing your charge amount on the payer’s allowed amount you may never see the incentive money that you have earned! Even a small percentage can add up quickly!
3. Decide on an Amount: If you aren’t sure where to start, consider setting your charge amounts based on the Medicare allowed amounts. Using 150% of the Medicare allowed amounts is a fairly standard starting point.
In addition to keeping the fee schedule current, make sure to monitor Allowed Amount and Paid Amount on a monthly basis. If you find that you are collecting the full allowed amount, it is time to increase the charge amount so you don’t leave money on the table!
If you need help getting started, consider working with a consultant. At RCM Insight, we offer annual fee schedule reviews. During the month of February 2021, we will be offering four practices a FREE fee schedule review, so visit our website at www.rcminsight.com and visit the CONTACT US page for your chance to win!
RCM Insight uses EZClaim’s medical billing software for their billing services. For more details about EZClaim’s medical billing solutions, visit their website, e-mail their support team, or call them at 877.650.0904.
[ Contribution: Stephanie Cremeans with RCM Insight ]