Sep 10, 2020 | Electronic Billing, Medical Billing Software Blog
So, it looks that there will be a lot new for E/M coding (Evaluation and Management) in 2021, and practices should start to get ready for it.
Well, it seems the only constant in the world of medical billing changes, and 2020 would only compliment that cliché. While the chaos of COVID-19 forced many unexpected changes—how you see your patients and bill for services—a bigger change is in the works for 2021. This change will complement the “Patients Over Paperwork” initiative from CMS and the AMA, which has been developed to eliminate “Note Bloat.” So, since the new year will roll out changes to E/M visits, now is the time to make sure that all parties are prepared for this long overdue and welcome change to medical billing.
Evaluation and management services have been long overdue for an overhaul. The 1995/1997 guidelines were in place well before electronic medical records, and with the growth of EMR’s, the process to document for a specific level required a lot of tedious, unnecessary documentation. (A cursory look at some of the proposed updates for E/M CPT coding and documentation requirements will verify that!)
PROPOSED CHANGES:
• History and Examination: While the elements of history and examination that are pertinent to a specific visit shall be recorded, they will no longer be used to ‘score’ the level billed
• Code Selection: It will be based on MDM or time
• Medical Decision Making: It will still utilize the CMS Table of Risk. However, the wording and explanations are being updated to provide more concise language. For instance, definitions will now be included to clearly identify subjective wording like “self-limited and stable chronic illness.” The clinical example will likely be removed, and the terms are more clearly defined. We will see this same type of clarification in the MDM table. For example, the 2021 guidelines will specify that the amount and/or complexity of data to be reviewed must also include analysis.
• Time-based Code Selection: It will also be easier. The guidelines will give specific amounts of time rather than the generic estimate that we currently see attached to E/M codes. Another major advantage to the codes selected based on time, they will now include non-face-to-face services. There will also be additional add on codes—in 15-minute increments—if the time has been exceeded for the 99205 or 99215.
While changes are daunting, this change will be rewarding from a documentation standpoint. So, if you need help with training your team on these new updates, there are FREE videos available on the AMA website, or you can enlist the help of an independent consultant like RCM Insight.
One way of keeping up with these changes is to use EZClaim’s medical billing software, which is continually updated. For more details, visit their website, ezclaim.com, contact them, or just give them a call at 877.650.0904.
[ Written by Stephanie Cremeans of EZClaim ]

Aug 11, 2020 | BillFlash, Partner, Revenue
Educating patients about their payment options can improve your medical practice revenue.
Imagine for a moment that you are planning to buy a car. Before you even enter a car lot, you do some research on the type of car you need, the features you are looking for, and how much you are able to spend. You might even get an opinion from a friend or check out reviews online.
After you have gathered all the information you need, you feel you are ready to start shopping—and confident that you might even get some new keys by the end of the day.
This is very similar to how most business transactions work: They have a need, they research the best ways to meet their need, and they make a purchase.
However, the healthcare industry doesn’t follow this formula. Your medical practice is a business just like any other, but your customers—aka, patients—often seek out your services not knowing exactly what they will be “buying” from you, nor how much they will be paying. Add in health insurance and surprise bills and you have a confusing hodgepodge of information that calculates the patient’s final bill, which they likely will not see for several weeks.
The current system is inefficient, and it is part of the reason that up to 30% of patient bills go unpaid every year.
Changing the Patient’s Financial Experience
Many practices have improved their revenue flow by simply treating their patients more like customers. In other words, they educate them on the financial side of things, as well as how to manage their health.
In a recent NexTrust webinar, three-quarters of poll respondents (doctors and practice managers) said that they speak to patients about their payment options. Thirty-one percent said that they currently use electronic communications, and only 8% use printed materials (flyers, signs, etc.).
While speaking to patients is a good start, getting payment information in writing is crucial to driving this information home. Patients already have a lot to remember regarding their care. A simple handout on how and when to make their payments can make it much easier for patients to manage their payment responsibility.
Most providers—over 90%—educate patients about how to pay on their statements. It certainly doesn’t hurt to communicate this information this way, but don’t rely on it exclusively. Most people skim the statement to see how much they owe and most miss important instructions.
So, as you educate patients on their payment options, keep these four key areas in mind to improve your medical practice revenue:
1) Set Clear Expectations about Payments
The first step in financially engaging your patients is to remind them you are a business, and that you require regular, on-time payments to keep your doors open. Patients often don’t see their doctors as business owners. A simple statement upfront about your payment expectations encourages patients to be more proactive about paying their bills on time.
2) Educate Patients about Your Payments Process
When patients understand your payments process, they are empowered to be more proactive in participating in it. You know where billing and payments fit into your practice workflow, so make sure patients understand that, too. If you require copays to be paid before a visit, communicate that beforehand so they can be prepared. In addition to that, also communicate clearly about when any remaining balances are due.
3) Push Your Online Payment Options
The best thing you can do to increase payments is to educate patients about their online payment options. Don’t just say “We accept payments online” and leave it at that. Show them where to go to complete payments. Also tell them about the variety of payment options available to them.
For example, EZClaim customers have several online payment options:
• Guest Pay: Patients can quickly pay their balance without having to set up an account
• MyProviderLink.com: If the patient wants access to more features (such as the ability to check their balance without having to call the office or to set up automatic payments), they can register for an account through BillFlash’s payment portal
• LinkPay: The practice sends a payment link to the patient before their visit, so they can pay what they owe before the visit starts
• PlanPay: Split up larger bills into smaller monthly payments
Online payments are the future of healthcare. So, make sure your online payment options are front and center whenever you bill patients. This could include a note in their statement directing them to pay online, handing out instruction cards on how to pay online, and posting signs throughout your office directing patients to your payment portal.
4) Reach Out to Patients You Haven’t Seen Lately
Forty percent of patients defer or skip care because they don’t think they can afford it. Make sure you get the word out to your entire patient base that you can accommodate any patient’s financial circumstances, whether that means setting up a payment plan or delaying payment for a few months. If patients know they have affordable payment options, they will be more likely to seek you out when they need help, rather than going somewhere else or deferring care entirely.
Empowering Patients to Take Ownership Over Their Healthcare Bills
Most patients want to pay their medical bills promptly and in full, but being in the dark about what they are being charged for and what their payment options are makes that difficult. The patient financial experience matters, and when you educate your patients on their online payment options and are transparent about costs, they usually respond positively, and you will improve your medical practice revenue.
Learn more about the pay services available to EZClaim customers by visiting their partner’s website, BillFlash.com, or by e-mailing sales@billflash.com.
To learn more about EZClaim’s medical billing software solution, visit their website at EZClaim.com.
[ Written by Angela Carter with BillFlash ]

Aug 11, 2020 | Features, Medical Billing Customer Service, Partner
Which is the BEST kind of Medical Billing Software? “All-in-One” or “Specialized”?
When considering WHICH medical billing solution they should use, practices wonder which is best, an “all-in-one” solution or specialized software. Well, the following are a few important pros and cons to consider when making a choice between these solutions.
ALL-IN-ONE:
An “all-in-one” system tries to provide a single, comprehensive solution that offers functionality for the major areas of the practice—Practice Management (PM), Electronic Medical/Health Records (EMR/EHR), and Revenue Cycle Management (RCM)—accessed from one central point. It has features like clinical notes, patient information, and history, diagnosis and treatments, scheduling, appointment reminders, reports, patient educational resources, as well as a medical billing section.
PROS:
• Most of what a practice need is included in the system
• There is no need to be concerned with multiple integrations or vendors
CONS:
• Tends to have a higher ‘entry’ cost
• Usually designed for the “middle-of-the-road,” therefore sometimes doesn’t properly address specific needs of a practice
• Sometimes, the practice is left paying for additional customizations to fit their particular needs
SPECIALIZED SOFTWARE:
Specialized medical billing software, on the other hand, is particularly programmed to maintain billing details of tests, procedures, examinations, diagnoses, and treatments conducted on patients. However, many specialized software providers extend their scope to include features like practice management, scheduling, and other administrative and clinical functions (that are generally a part of EHR software systems) by partnering with other specialty software companies—creating a “best-in-class” solution.
PROS:
• Integrating multiple “best-in-class” software packages—each taking a much more focused approach—creates an offering with much more in-depth capabilities
• Usually are more ‘nimble’ in responding to industry and regulatory changes
• More ’scalable’ in supporting the growth of a practice
CONS:
• Most of the time the practice has to deal with multiple vendors
CONCLUSION:
Where “all-in-one” solutions offer a wide breadth of capabilities across the business, they usually also lack focus, depth, and sophistication. “All-in-one” solutions are usually only efficient in one area, with the other areas tend to be ‘compromised’ and not fully developed. Then, when it comes to flexibility, they tend to be slow to adapt to changing practice needs.
Specialized software, however, typically offer a more efficient experience, with each ‘component’ streamlined and designed with a specific purpose in mind. Their focus on limiting the software scope makes them flexible and easy to use.
EZClaim—a leading software package in medical billing and practice management—has made it easier for the medical practice to have the benefit of a “all-inclusive” solution. They have created the best of both worlds by taking on the responsibility of integrating the “best-of-breed” into a harmonized “best-of-class” offering that allows the practice to pick and choose for their specific needs. The seamless integration of partner products and services ensures the practice does not have to give up robustness and flexibility for a simplified “all-in-one” solution, and it further enhances the practice’s workflow.
As a specific example, one of EZClaim’s partners is TriZetto Provider Solutions (TPS), a provider that seamlessly blends claims processing with revenue management and analytics software, so the practice can get paid faster, and more accurately.
Today, the practice can get the benefit of all the power and ease of use of EZClaim’s medical billing software and all the access and security that is needed when dealing with personal records by using TPS—which includes patient access, claims and denials management, patient financials, and advisory services.
The powerful integration between EZClaim and TPS efficiently adds functionality to the practice. Now the practice can gain deeper insight into the claim lifecycle, and take the proper steps to improve the overall health of the practice. The right ‘integrated’ solution makes all the difference!
So, if your practice needs more confident billing, after payments, and more informed decisions, but the power of EZClaim and TPS to work for your practice with the integrated suite of revenue cycle solutions.
In addition to TPS, EZClaim has tightly integrated a variety of of ‘components’ to be able to offer an “all-inclusive” best-in-class solution for a medical practice’s needs: Electronic Health Records (EHR), Clearinghouse, statement and payment services, HIPPA compliance, claims scrubbing, appointment reminders, and inventory management. It has partnered with a variety of providers like QuickEMR, BestNotes, and PracticeFusion [ Click here for an entire list of EZClaim’s partners ].
It is important to note that an “all-in-one” solution does not usually include the Clearinghouse portion that TPS offers. The powerful integration between EZClaim, TPS, and EZClaim’s EMR partners, efficiently adds functionality to ANY practice!
If you are considering the best course of action to meet your practice’s needs, consider using EZClaim by downloading a FREE TRIAL or contact one of their product specialists today to explore all the options for how to best solve your practice’s operational challenges, and grow your business.
For details and features about EZClaim’s medical billing software, visit their website.
Jul 14, 2020 | Health eFilings, MIPS Reporting, Partner, Revenue
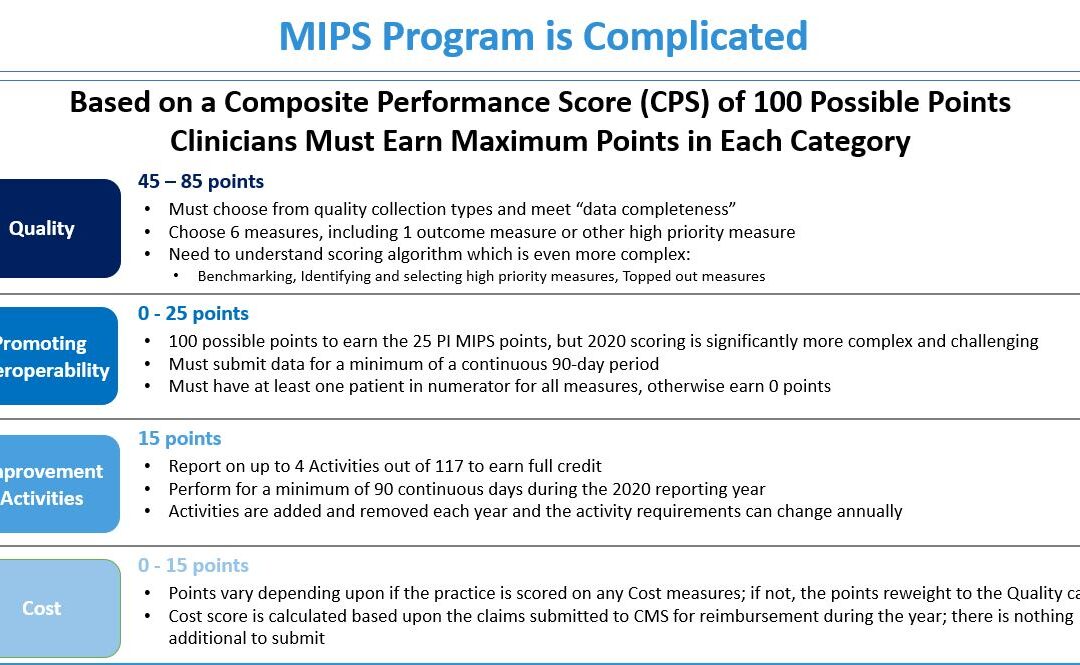
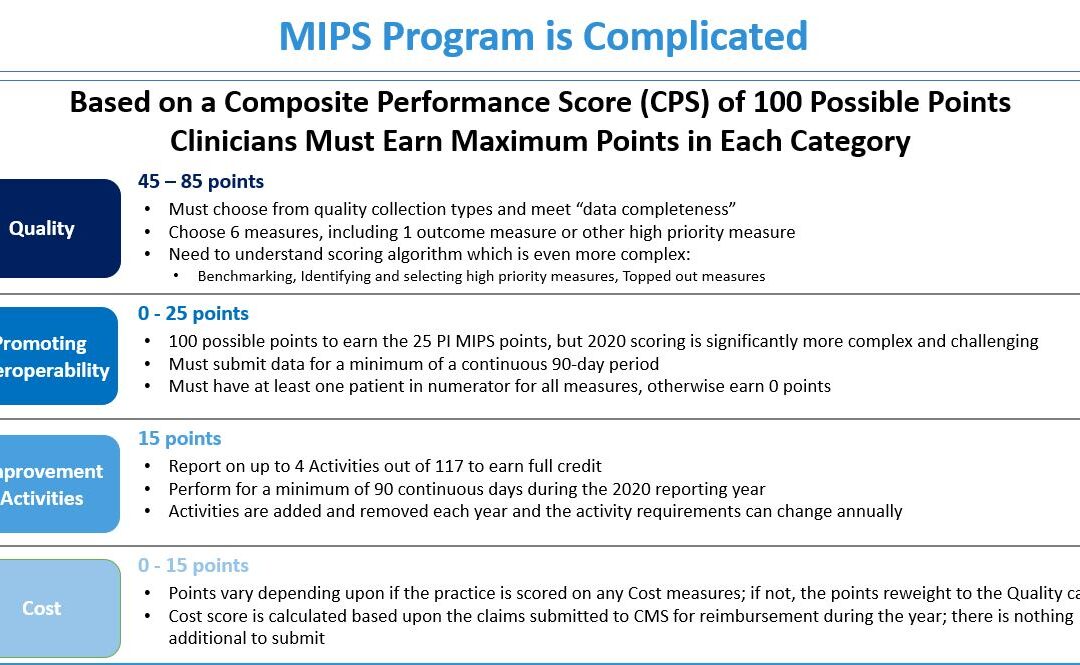
The 2020 MIPS reporting is already half done, and given that MIPS (Merit-based Incentive Payment System) is a points-based program, the goal is to earn as many points as possible to avoid this year’s 9% penalty and potentially even earn a positive payment adjustment. However, earning the 45 points necessary to avoid the penalty for the 2020 reporting period will be no easy feat. With over half of the reporting period already behind us, it is imperative you ACT NOW so you don’t find yourself in a position later in the year that you can’t recover from in terms of earning points.
With all the complexities and nuances of the program, it’s challenging to know what you can do to impact your score. Here are three critical actions to take right now so that you will still optimize your ability to earn points for the 2020 reporting period:
1. Focus on the Quality Category
There are various points available within each of the categories and the Quality Category has the most points associated with it. Based on a number of factors, the category is worth anywhere from 45 to 85 points. This is a critical category to be focused on throughout the year, so now is the time to ensure that you are tracking all relevant data so that it can be properly reported on within your submission.
2. Understand the Timeframe Requirements
Two of these categories, Promoting Interoperability and Improvement Activities, have timeframe requirements where you must perform for a minimum of 90 continuous days. These are not easy categories in which to be successful and so if you wait too long in the year you will find it impossible to put the right actions in place in order to complete the activities necessary to earn any of the points in these categories.
3. Choose the Right Reporting Methodology
Not all reporting methodologies are the same and the reporting methodology you select has a significant impact on the points you could earn. Additionally, there is strategic maneuvering that can be done throughout the reporting period with exemptions and reweighting of points that can set you up to optimize your performance and your score. Therefore, you must select a reporting partner that will help you earn the most points available and leverages technology to facilitate the ease, accuracy, and completeness of tracking and reporting to maximize your score. Reporting via a CEHRT, like Health eFilings, is the best approach because it optimizes the points that could be earned and therefore, maximizes Medicare reimbursements.
Health eFilings is a certified EHR technology (CEHRT) and the national leader in automated MIPS reporting. Their cloud-based ONC-certified software fully automates the reporting process. Because Health eFilings’ service is an end-to-end electronic solution that doesn’t require any IT resources, administrative support, or workflow changes from you, the practice will save significant time while maximizing its financial upside.
To learn more about how to properly perform your 2020 MIPS reporting, contact EZClaim’s partner, Health eFilings, so they can help before it’s too late!
For details and features about EZClaim’s medical billing software, or general information about the company, visit their website.
[ Written by Sarah Reiter, SVP Strategic Partnerships, Health eFilings ]

Jul 14, 2020 | Alpha II, MIPS Reporting, Partner, Webinar
Join this MIPS Reporting Webinar to be sure you are up to speed on the latest updates and changes.
Now that the MIPS (Merit-based Incentive Payment System) submission period is drawing to a close, join our partner, Alpha II, as they review the updates and changes for MIPS reporting in 2020. This session will discuss important program updates for 2020 reporting including:
• Eligibility requirements
• Performance thresholds
• Payment adjustments
• Performance category weighting
• Measure updates and more…
MIPS Reporting Webinar details:
Start reporting correctly now to ensure success for the 2020 performance year!