Optimize your MIPS Score and Protect your Reimbursements
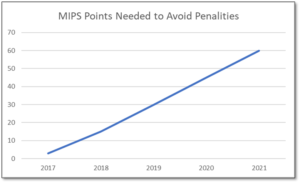
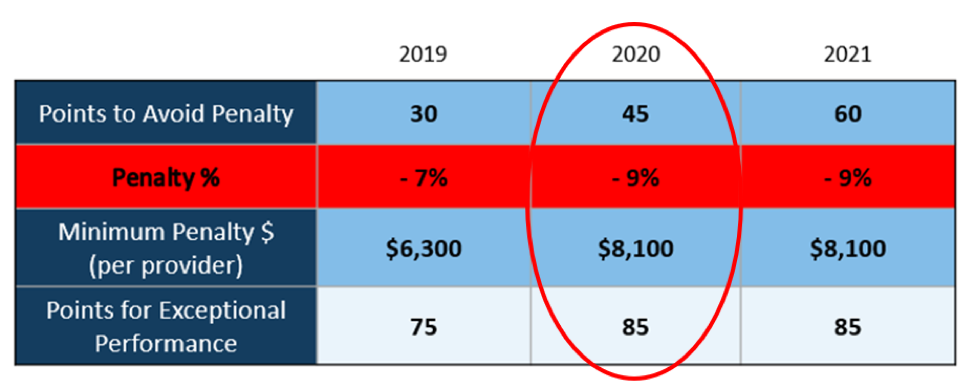
MIPS is a point-based program and understanding how to earn MIPS points is critical to avoid a 9% penalty. The MIPS program continues to change and evolve each year as it meets the goals laid out in the MACRA law and carried out by CMS. Since the program was implemented in 2017 the points threshold to avoid a penalty has grown from 3 to 60 out of a possible 100 MIPS points; the penalty has increased from 3% to 9% of annual Medicare reimbursements; and, the number of patients required to be reported on has increased from 20 patients to all patients for all payors. With the rules changing every year, the strategy you previously used to score MIPS points and report may no longer be optimal. If you want to avoid the 9% penalty in 2021 and beyond, you must think differently and evolve your strategy for MIPS.
With all the complexities and nuances of the program, it’s challenging to know what you can do to impact your MIPS score. Here are three critical considerations that provide guidance on ensuring you have the right MIPS strategy to optimize your ability to earn MIPS points for the 2021 reporting period.
The Quality Category, worth the most points, is the category to focus most of your effort. Because the Quality category is worth anywhere from 40 to 85 MIPS points, focusing on this category throughout the year is critical. You need to submit a full year’s worth of data so now is the time to ensure that you are capturing all relevant data in your EHR and or billing system so that it can be properly extracted and reported on for your submission.
40% of the MIPS points require you meet stringent timeframe requirements. Two of the MIPS categories, Promoting Interoperability and Improvement Activities, have timeframe requirements where you must perform and document activities for a minimum of 90 continuous days. These are not easy categories in which to be successful and so if you wait too long you will find it impossible to put the right actions in place to complete the activities necessary to earn any of the MIPS points in these categories.
The reporting methodology you choose impacts the points you can earn. Not all reporting methodologies are the same and the reporting methodology you select has a significant impact on the MIPS points you could earn. Unless you select a reporting partner that will help you earn the most points available by leveraging technology to facilitate the ease, accuracy, and completeness of tracking and reporting to maximize your score, you risk leaving MIPS points on the table and significantly sub-optimizing your score. Reporting via a CEHRT, like Health eFilings, is the best approach because it optimizes the MIPS points that could be earned and therefore, maximizes Medicare reimbursements.
Health eFilings’, a CEHRT, is the national leader in automated MIPS reporting and our cloud-based ONC certified software fully automates the MIPS reporting process. And because Health eFilings’ service is an end-to-end electronic solution that doesn’t require any IT resources, administrative support, or workflow changes, you will save significant time while maximizing your financial upside.
Contact Sarah Reiter, sreiter@healthefilings.com, or 608.841.1866 to find out how to maximize your reimbursements and protect your bottom line.
About Health eFilings:
Health eFilings, a CEHRT, is the national leader in automated MIPS compliance and quality data analytics. Its services drive improved patient outcomes, optimized quality measures, and stronger financial results for healthcare practices. Their proprietary cloud-based ONC certified software is significantly more efficient and effective than any registry as it does all the work to extract, calculate, benchmark, format, and electronically submit MIPS data to CMS so clients avoid significant penalties and earn maximum reimbursements. And, you can have peace of mind knowing you are working with the best partner because CMS has accepted 100% of Health eFilings’ submissions. Learn more here: https://healthefilings.com/ezclaim
ABOUT EZCLAIM:
EZClaim is a leading medical billing and scheduling software provider that combines a best-in-class product, with correspondingly exceptional service and support. For more inforatmion, schedule a consultation today, email our experts, or call at 877.650.0904.