May 12, 2022 | Health eFilings, Partner
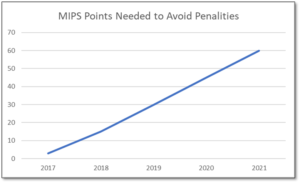
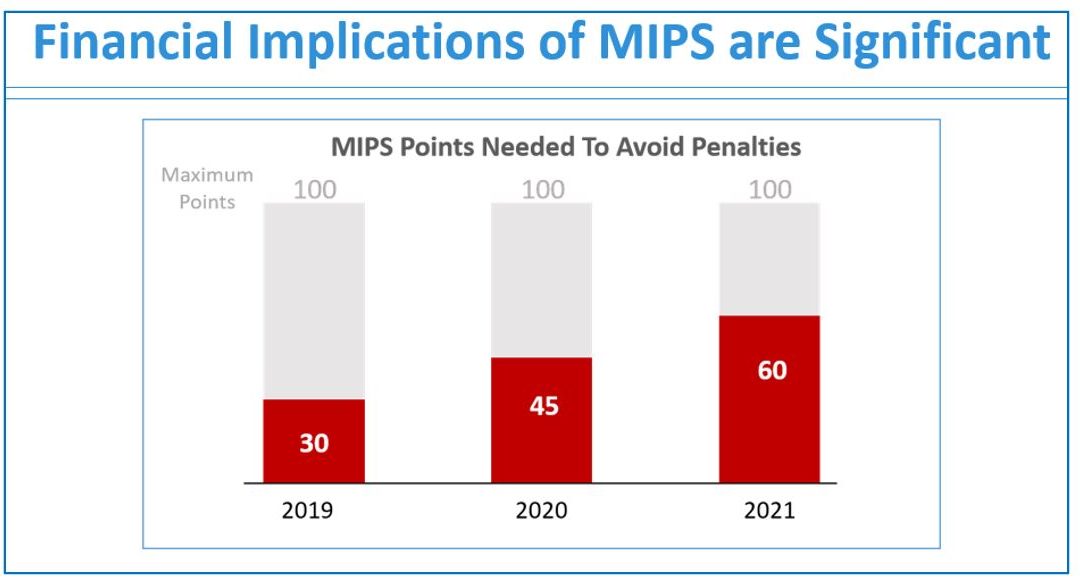
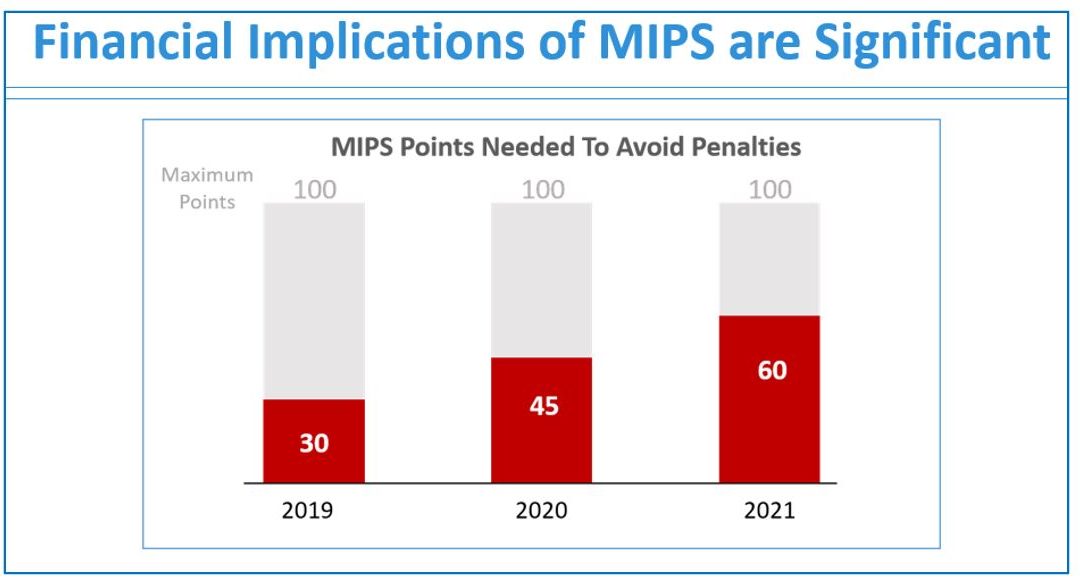
MIPS is a point-based program and understanding how to earn MIPS points is critical to avoid a 9% penalty. The MIPS program continues to change and evolve each year as it meets the goals laid out in the MACRA law and carried out by CMS. Since the program was implemented in 2017 the points threshold to avoid a penalty has grown from 3 to 60 out of a possible 100 MIPS points; the penalty has increased from 3% to 9% of annual Medicare reimbursements; and, the number of patients required to be reported on has increased from 20 patients to all patients for all payors. With the rules changing every year, the strategy you previously used to score MIPS points and report may no longer be optimal. If you want to avoid the 9% penalty in 2021 and beyond, you must think differently and evolve your strategy for MIPS.
With all the complexities and nuances of the program, it’s challenging to know what you can do to impact your MIPS score. Here are three critical considerations that provide guidance on ensuring you have the right MIPS strategy to optimize your ability to earn MIPS points for the 2021 reporting period.
The Quality Category, worth the most points, is the category to focus most of your effort. Because the Quality category is worth anywhere from 40 to 85 MIPS points, focusing on this category throughout the year is critical. You need to submit a full year’s worth of data so now is the time to ensure that you are capturing all relevant data in your EHR and or billing system so that it can be properly extracted and reported on for your submission.
40% of the MIPS points require you meet stringent timeframe requirements. Two of the MIPS categories, Promoting Interoperability and Improvement Activities, have timeframe requirements where you must perform and document activities for a minimum of 90 continuous days. These are not easy categories in which to be successful and so if you wait too long you will find it impossible to put the right actions in place to complete the activities necessary to earn any of the MIPS points in these categories.
The reporting methodology you choose impacts the points you can earn. Not all reporting methodologies are the same and the reporting methodology you select has a significant impact on the MIPS points you could earn. Unless you select a reporting partner that will help you earn the most points available by leveraging technology to facilitate the ease, accuracy, and completeness of tracking and reporting to maximize your score, you risk leaving MIPS points on the table and significantly sub-optimizing your score. Reporting via a CEHRT, like Health eFilings, is the best approach because it optimizes the MIPS points that could be earned and therefore, maximizes Medicare reimbursements.
Health eFilings’, a CEHRT, is the national leader in automated MIPS reporting and our cloud-based ONC certified software fully automates the MIPS reporting process. And because Health eFilings’ service is an end-to-end electronic solution that doesn’t require any IT resources, administrative support, or workflow changes, you will save significant time while maximizing your financial upside.
Contact Sarah Reiter, sreiter@healthefilings.com, or 608.841.1866 to find out how to maximize your reimbursements and protect your bottom line.
About Health eFilings:
Health eFilings, a CEHRT, is the national leader in automated MIPS compliance and quality data analytics. Its services drive improved patient outcomes, optimized quality measures, and stronger financial results for healthcare practices. Their proprietary cloud-based ONC certified software is significantly more efficient and effective than any registry as it does all the work to extract, calculate, benchmark, format, and electronically submit MIPS data to CMS so clients avoid significant penalties and earn maximum reimbursements. And, you can have peace of mind knowing you are working with the best partner because CMS has accepted 100% of Health eFilings’ submissions. Learn more here: https://healthefilings.com/ezclaim
ABOUT EZCLAIM:
EZClaim is a leading medical billing and scheduling software provider that combines a best-in-class product, with correspondingly exceptional service and support. For more inforatmion, schedule a consultation today, email our experts, or call at 877.650.0904.

Nov 11, 2021 | Health eFilings, Partner
MIPS Strategic Guide – How to Choose the Right Reporting Partner
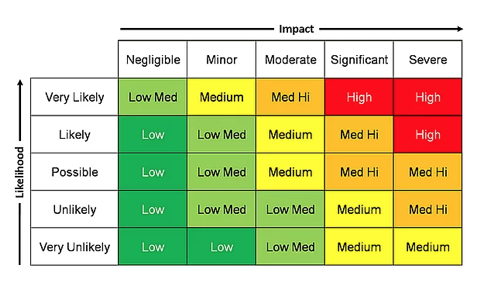
Given the way the MIPS program has evolved, all healthcare practices regardless of size or specialty must evolve their approach to MIPS reporting to assure their success with the program. However, most clinicians do not understand or don’t have awareness of, the different reporting methods available to them and the impact the reporting method can have on their success with MIPS. With what is at stake financially, it is critical that you understand and select the right methodology and partner to maximize your MIPS points and protect your bottom line.
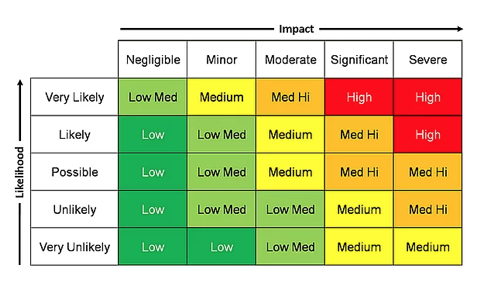
Many clinicians erroneously think that a registry is the only reporting option available to them or that they are required to use a registry. Or, they think that their EHR handles reporting for them. These misperceptions and general lack of awareness of the other reporting methodology will be detrimental to your ability to be successful with MIPS. And, given that 50% of all clinicians will be penalized annually by next year, the legacy reporting methods (registry or EHR) will not be able to fulfill enough of the reporting criteria to earn the minimum MIPS points needed to avoid the 9% reduction in Medicare reimbursements.
To help you determine if you are choosing the right reporting method and partner, we’ve identified the five most important factors to consider in order to increase your probability of avoiding the 9% penalty.
- Reporting Classification – is the reporting partner a CEHRT?
- Service Approach — Does the reporting partner use ONC certified software to do all the work with no IT resources, administrative support, or workflow changes?
- Quality Measures — Is the reporting partner certified by CMS to calculate all eCQMs, which earn significantly more points than registry measures?
- Benchmarking — Are proprietary algorithms used to assess the 9 million possible combinations of Quality measures to maximize earning MIPS points?
- Submission Method — Does the reporting partner submit a comprehensive electronic file directly to CMS to comply with reporting for all MIPS categories?
If you answer “no” to any of these questions, then the reporting partner you are working with will not be able to maximize the MIPS points you can earn. Given every MIPS point matters, because MIPS points determine your reimbursements and impact your bottom line, it’s time to consider a new strategy with a new reporting partner.
Health eFilings, a CEHRT, is the national leader in automated MIPS reporting. They utilize ONC-certified software to handle 100% of the tracking and reporting of the required data to CMS. And because their service is classified as an end-to-end electronic solution, you’ll also earn additional bonus points toward your MIPS score even though they are doing all the work. Health eFilings as your partner is the more effective and efficient reporting method so you will earn more points and, ultimately, receive higher reimbursements.
Learn more about how Health eFilings can help your practice here: https://healthefilings.com/ezclaim. Contact Sarah Reiter, sreiter@healthefilings.com, or 608.841.1866 to find out how to maximize your Medicare reimbursements and protect your bottom line.
About Health eFilings:
Health eFilings, a CEHRT, is the national leader in automated MIPS compliance and quality data analytics. Its services drive improved patient outcomes, optimized quality measures, and stronger financial results for healthcare practices. Their proprietary cloud-based ONC certified software is significantly more efficient and effective than any registry as it does all the work to extract, calculate, benchmark, format, and electronically submit MIPS data to CMS so clients avoid significant penalties and earn maximum reimbursements. And, you can have peace of mind knowing you are working with the best partner because CMS has accepted 100% of Health eFilings’ submissions. Learn more here: https://healthefilings.com/ezclaim
ABOUT EZCLAIM:
As a medical billing expert, EZClaim can help the medical practice improve its revenues since it is a medical billing and scheduling software company. EZClaim provides a best-in-class product, with correspondingly exceptional service and support. Combined, EZClaim helps improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.
Jan 11, 2021 | Electronic Billing, Health eFilings, Medical Billing Software Blog, Partner
If you are not a MIPS expert (Merit-based Incentive System), your Medicare reimbursements may be decreased by 9% in the next year. However, it’s not too late to avoid the penalty for the 2020 reporting period, but you need to act now!
One of EZClaim’s partners, Health eFilings’ has ONC-certified software that completely automates the MIPS compliance process for you. The software will automatically extract the required data directly from EZClaim (and/or your EHR), and then proprietary algorithms will process the 9,000,000 possible combinations of quality measures for each clinician to identify which measures should be submitted to CMS (Centers for Medicare and Medicaid Services) to earn you the most points.
Need a MIPS expert? Well, Health eFilings is one of the best, and CMS has accepted 100% of their submissions on behalf of their clients. If you have completed your 2020 reporting, reach out to them, and learn how you can earn even more points in 2021.
For more information about EZClaim’s medical billing software, e-mail, visit their website, or contact them at 877.650.0904.
[ Article contributed by Sarah Reiter, SVP Strategic Partnerships, Health eFilings]

Oct 13, 2020 | Health eFilings, Webinar
This FREE Medicare reimbursements webinar will help healthcare providers with the financial challenges they are facing this year, and it’s critical not to ignore the impact MIPS compliance has on their bottom line.
There are many commonly misunderstood aspects of MIPS (Merit-based Incentive Payment System), and many nuances of how and when actions need to be taken to be able to earn points—and points significantly impact reimbursements!
To help bring clarity to MIPS, Health eFilings is holding a FREE 30-minute Medicare reimbursements webinar to help you understand key deadlines for this reporting period, what reporting methods will optimize your MIPS score, and how to increase the financial payouts from the MIPS program.
• Date: TUESDAY, DECEMBER 8, 2020, 1:00 – 1:30 pm EST
• Presenter: SARAH REITER, SVP Strategic Partnership of Health eFilings
• Register Here: https://healthefilings.com/ezclaim
The 2020 reporting period is quickly coming to a close, but there is still time to comply and avoid penalties. However, you must act quickly, so Health eFilings is here to help: https://healthefilings.com/ezclaim

Health eFilings is a ‘partner’ of EZClaim, a medical billing and scheduling software solution. For more details about their software, visit their website: ezclaim.com/features-pricing/
Oct 13, 2020 | HIPAA, Live Compliance, Medical Billing Software Blog, Partner
New HIPAA compliance requirements are coming!
In an effort to make the HIPAA Privacy Rule as easy to understand as possible, the Office for Civil Rights (OCR) has come up with a list of rules that clearly explain what Business Associates are now “directly liable” for. As OCR Director Roger Severino explains, “We want to make it as easy as possible for regulated entities to understand, and comply with, their obligations under the law.” The list consists of ten rules that, if failed to follow, can result in penalties and monetary fines.
[ Note: Check out our previous post to access this list ].
Immediate Requirements:
As we enter the fourth quarter of the year, you may be wondering what immediate requirements should a Business Associate complete before the end of the year?
One of the most important rules also includes information about Business Associates, and their need for proof of satisfactory assurance when the covered entity requests this of them. Satisfactory assurance is crucial, because it ensures the Business Associate is HIPAA compliant, and therefore, must also be in the form of a contract.
The Satisfactory Assurance contract is oftentimes outlined in the form of a questionnaire, and requires the Business Associate to disclose the date of completion for various compliance requirements.
These include distribution and completion of workforce HIPAA training, implementation and distribution of policies and procedures, Business Associate documentation, and completion of an annual HIPAA Security Risk Assessment.
Are You Prepared?:
If a Covered Entity requests this proof from your organization, would you be able to successfully complete it without outdated completion?
If you are uncertain that your organization would be able to easily and efficiently provide that documentation, you may be facing thousands of dollars in fines for each vulnerability!
HIPAA Compliance Myths:
False: The security risk analysis is optional for small providers: All providers who are “Covered Entities” under HIPAA are required to perform a risk analysis. In addition, all providers who want to receive MU, and MIPS incentive payments must conduct a risk analysis.
False: Our office uses the Cloud, so we don’t need a risk assessment: Even if you have a fully HIPAA compliant cloud vendor, your patient data (ePHI and PII) still must go through all your systems to get to the cloud. So, you are still required to perform technical, administrative, and physical security risk analyses.
False: Our EHR makes us compliant, so we’re fine: While your EHR may provide excellent privacy and security features, it definitely doesn’t exempt you from the HIPAA security requirements.
Live Compliance helps their clients meet the ever changing and complex HIPAA State and Federal regulations. They protect the information they are entrusted with, and ensure their clients pass any Health and Human Services audits. If you are unsure or need assistance, call Jim Johnson with Live Compliance at (980) 999-1585.
Live Compliance is a partner of EZClaim, a medical billing software company. For more details about their solutions, visit their website at ezclaim.com.