Jul 14, 2020 | Health eFilings, MIPS Reporting, Partner, Revenue
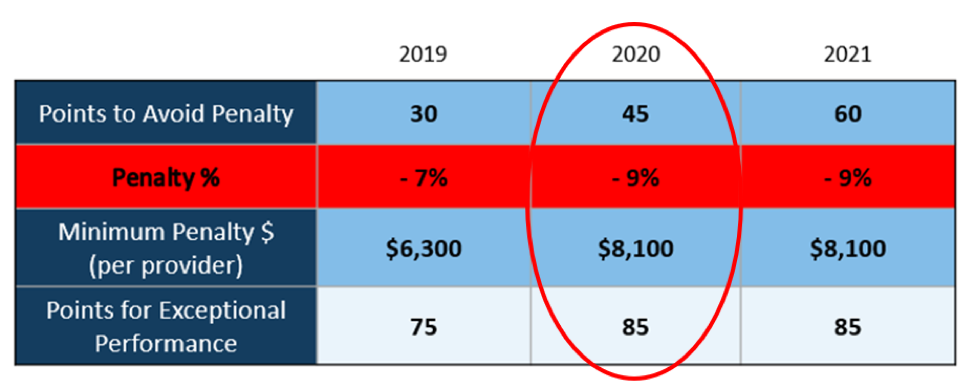
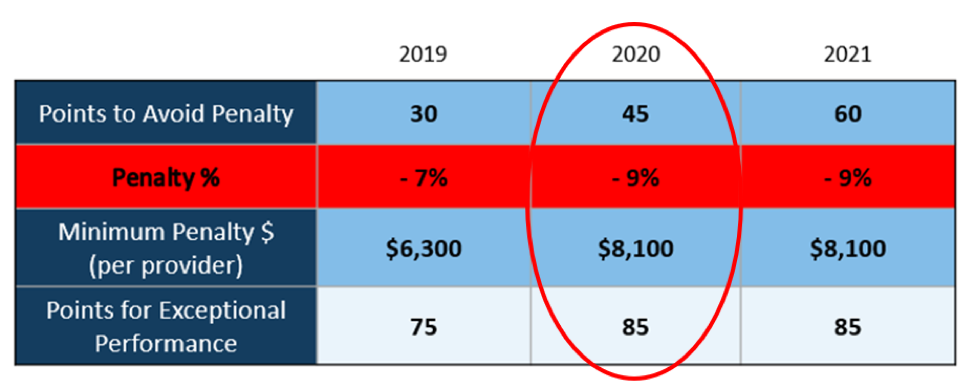
The 2020 MIPS reporting is already half done, and given that MIPS (Merit-based Incentive Payment System) is a points-based program, the goal is to earn as many points as possible to avoid this year’s 9% penalty and potentially even earn a positive payment adjustment. However, earning the 45 points necessary to avoid the penalty for the 2020 reporting period will be no easy feat. With over half of the reporting period already behind us, it is imperative you ACT NOW so you don’t find yourself in a position later in the year that you can’t recover from in terms of earning points.
With all the complexities and nuances of the program, it’s challenging to know what you can do to impact your score. Here are three critical actions to take right now so that you will still optimize your ability to earn points for the 2020 reporting period:
1. Focus on the Quality Category
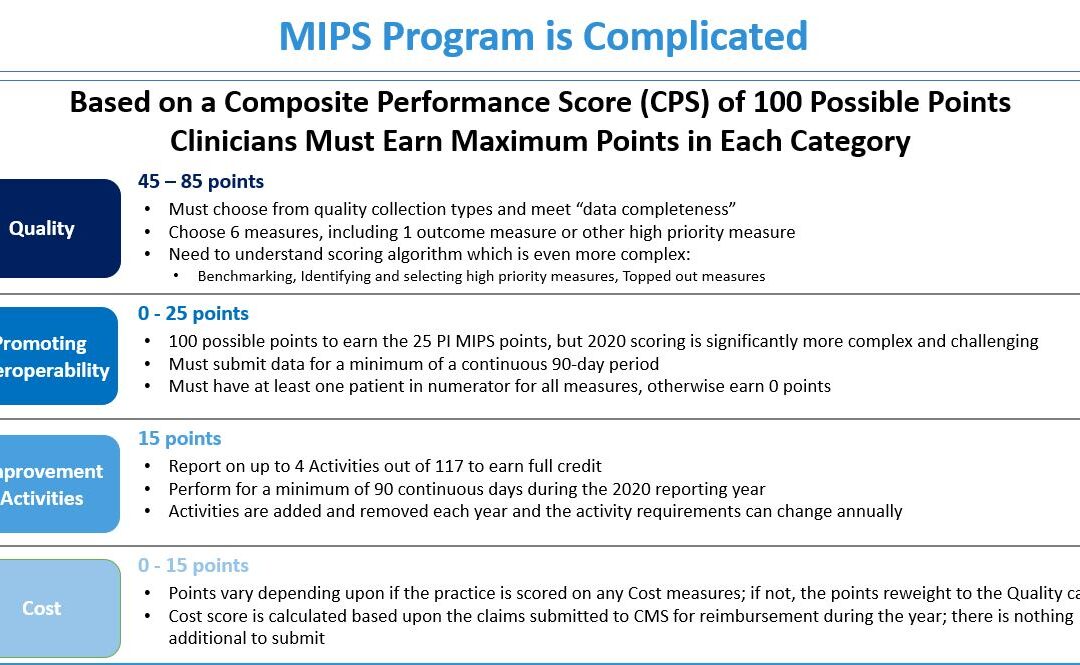
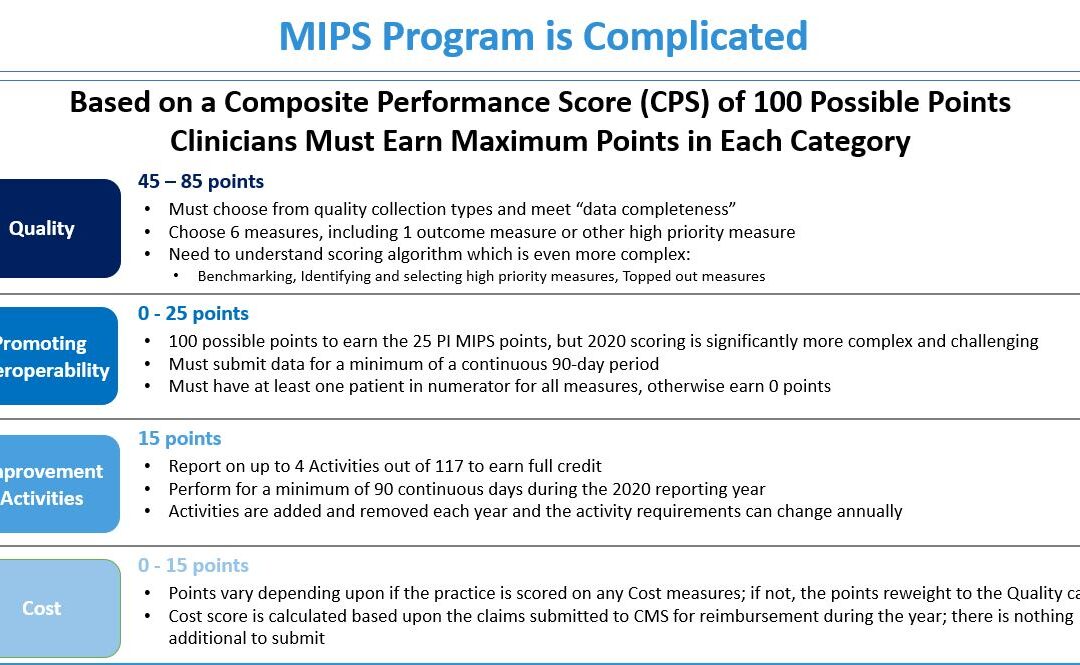
There are various points available within each of the categories and the Quality Category has the most points associated with it. Based on a number of factors, the category is worth anywhere from 45 to 85 points. This is a critical category to be focused on throughout the year, so now is the time to ensure that you are tracking all relevant data so that it can be properly reported on within your submission.
2. Understand the Timeframe Requirements
Two of these categories, Promoting Interoperability and Improvement Activities, have timeframe requirements where you must perform for a minimum of 90 continuous days. These are not easy categories in which to be successful and so if you wait too long in the year you will find it impossible to put the right actions in place in order to complete the activities necessary to earn any of the points in these categories.
3. Choose the Right Reporting Methodology
Not all reporting methodologies are the same and the reporting methodology you select has a significant impact on the points you could earn. Additionally, there is strategic maneuvering that can be done throughout the reporting period with exemptions and reweighting of points that can set you up to optimize your performance and your score. Therefore, you must select a reporting partner that will help you earn the most points available and leverages technology to facilitate the ease, accuracy, and completeness of tracking and reporting to maximize your score. Reporting via a CEHRT, like Health eFilings, is the best approach because it optimizes the points that could be earned and therefore, maximizes Medicare reimbursements.
Health eFilings is a certified EHR technology (CEHRT) and the national leader in automated MIPS reporting. Their cloud-based ONC-certified software fully automates the reporting process. Because Health eFilings’ service is an end-to-end electronic solution that doesn’t require any IT resources, administrative support, or workflow changes from you, the practice will save significant time while maximizing its financial upside.
To learn more about how to properly perform your 2020 MIPS reporting, contact EZClaim’s partner, Health eFilings, so they can help before it’s too late!
For details and features about EZClaim’s medical billing software, or general information about the company, visit their website.
[ Written by Sarah Reiter, SVP Strategic Partnerships, Health eFilings ]

Jul 14, 2020 | Alpha II, MIPS Reporting, Partner, Webinar
WEBINAR: Understanding QPP MIPS Measure Specifications
Hear it from the experts! Learn how to interpret Quality and Promoting Interoperability Measure Specifications from Alpha II’s Qualified Registry auditors.
They will reveal the most common mistakes found in quality reporting and show the importance of understanding your measures. Topics include:
• Understanding denominator exclusions
• Adding required denominator G-codes
• Visit requirements
• Importance of notes
• Numerator instructions
• Special numerator criteria such as minimum day requirements
• Promoting Interoperability measure requirements and more…
Understanding QPP MIPS Webinar details:
• Date: July 28, 2020 @ 1pm (EST)
• EZClaim Link: https://alphaii.zoom.us/webinar/register/2915940667921/WN_7pUJlJs3RGSytrMoNsrYJQ

Jul 14, 2020 | Alpha II, MIPS Reporting, Partner, Webinar
Join this MIPS Reporting Webinar to be sure you are up to speed on the latest updates and changes.
Now that the MIPS (Merit-based Incentive Payment System) submission period is drawing to a close, join our partner, Alpha II, as they review the updates and changes for MIPS reporting in 2020. This session will discuss important program updates for 2020 reporting including:
• Eligibility requirements
• Performance thresholds
• Payment adjustments
• Performance category weighting
• Measure updates and more…
MIPS Reporting Webinar details:
Start reporting correctly now to ensure success for the 2020 performance year!
Apr 13, 2020 | Health eFilings, Partner
There WILL NOT be any changes to the MIPS Program in 2020, so all payers must be submitted and a minimum of 45 points must be earned to avoid the 9% penalty.
On March 23, 2020, CMS made it perfectly clear that MIPS Program is not going away in 2020. It also reiterated that the data requirements and thresholds in place for the 2020 program have not changed. Additionally, Promoting Interoperability and Improvement Activities must be done for the required durations, or no points will be earned for those categories.
To put this in context, while the stakes have been raised every year, the final ruling for the 2020 reporting period is the most complex to-date, further increasing the stress, burden, and financial risk for over 900,000 clinicians who bill Medicare Part B. Failure to comply or earn enough points for the 2020 reporting period will result in an automatic 9% penalty on every Medicare Part B claim paid for an entire year. This equates to a minimum of a $8,100 per provider hit to the bottom line.
Given the unprecedented time when everyone’s bottom line is at risk, now is the time to get a handle on what’s at risk with the MIPS program and proactively engage to ensure your bottom line is not further jeopardized by being assessed a 9% penalty. It can be challenging to know exactly what you need to do to earn points, optimize your score, and protect your Medicare reimbursements, as there are many commonly misunderstood aspects and nuances with the MIPS program.
So, with what is at stake and the inherent complexity in earning points, it is critical that you select the right methodology and partner who can help you maximize reimbursements and protect your bottom line. Not all reporting methodologies are the same.
Health eFilings‘ CEHRT is the best choice for a reporting partner. Their cloud-based ONC-certified software fully automates the process and does all the work without any IT resources, administrative support, and workflow changes from the practice. Health eFilings service is an end-to-end electronic solution that will save significant time, be a turn-key submission process, and maximize the financial upside for providers.
As more than 25% of the 2020 reporting period is behind us, now is the time to act while there is still plenty of time to positively impact your results and points earned.
Health eFiling provides the nation’s only fully automated solution for MIPS compliance and is integrated with EZclaim’s billing solution. Click on the following link for more details: https://healthefilings.com/ezclaim
[Contribution by Sarah Reiter with the Senior VP of Strategic Partnerships]