Jan 11, 2021 | BillFlash, Medical Billing Software Blog, NexTrust, Partner
There are five primary medical practice fundamentals that, if focused on, will ensure your practice is working toward goals that will make the biggest difference. Practices are pulled in many directions each day, and it can be difficult to know what to prioritize, so the following are some recommendations.
1) Define Patient Engagement Goals
Perhaps one of the most overused terms in today’s medical field is “patient engagement.” Much like the drawer filled with important yet miscellaneous items, if you can’t actually define it, you probably aren’t going to do something with it.
In 2021, it is imperative to define your office’s patient engagement goals in order to determine whether they are being met, and more importantly, if the value you’ve placed on engagement is benefitting your bottom line. This could include engaging via a more personal checkout process that explains how billing and payment will be done and asking patients if there are certain times of the year they wish to be notified for annual wellness checks.
2) Ask For Online Reviews
Reviews remain one of the highest drivers of new customer acquisition. As a local business, you can create a Google Business account online that provides your address, phone number, and link to your website. Included is the ability to add reviews as well as phrases and keywords about your business within the Google Business dashboard, and it’s all free!
To encourage your patients to leave reviews, create cards with step-by-step instructions for posting online reviews via Google. Be picky. Make sure you ask your best patients to participate, who will be honored that you asked. Don’t forget to monitor to see how your business listing looks to potential new patients.
3) Offer Friendly Medical Bills
Of course, we’re not suggesting you add flowers or poignant sayings. Rather, explain a statement to your patients at checkout or within their financial package; this helps the process flow more naturally. BillFlash patient statements have five different messaging rows you can customize for communication. Plus, you can also send electronic patient statements through text and email.
In 2021, communication with patients—even on billing statements—should be natural, friendly, and simple. Getting paid is a segment of the medical practice workflow and should be as easy and frictionless as possible.
4) Ask About Payment Preferences
People are driven by routine and behavior. In today’s world, when paying for an item, the buyer is offered numerous options including cash, debit and credit, no-interest, pay-over-time plans, payment apps, or even Near Field Communication (NFC) like Apple and Google Pay. Granted, the last two have had very low adoption rates, but keeping an eye on payment trends costs little more than time and may add something unexpected to your bottom line.
In 2021, identifying the preferred patient payment options could be the difference between getting paid quickly and not getting paid at all. Don’t overlook the enormous value people place on how they give and take money.
5) Use RCM Services
An RCM vendor helps you get the most out of your practice revenue. They help you collect more from difficult balances, empower patients to pay in full, and improve your claims processing—without adding extra work for your office staff. Working with the right RCM services provider ensures you are paid more for the work you do. They also help identify reasons for claims denials, which have a positive impact on your practice revenue, as well.
For more information about automated patient statements and patient payment options, contact EZClaim, NexTrust BillFlash, GetPaid@BillFlash.com, or call BillFlash at 435.940.9123 (Option 3). For more details about EZClaim’s medical billing software, visit their website, e-mail their support team, or call them at 877.650.0904.

Aug 11, 2020 | Features, Medical Billing Customer Service, Partner
Which is the BEST kind of Medical Billing Software? “All-in-One” or “Specialized”?
When considering WHICH medical billing solution they should use, practices wonder which is best, an “all-in-one” solution or specialized software. Well, the following are a few important pros and cons to consider when making a choice between these solutions.
ALL-IN-ONE:
An “all-in-one” system tries to provide a single, comprehensive solution that offers functionality for the major areas of the practice—Practice Management (PM), Electronic Medical/Health Records (EMR/EHR), and Revenue Cycle Management (RCM)—accessed from one central point. It has features like clinical notes, patient information, and history, diagnosis and treatments, scheduling, appointment reminders, reports, patient educational resources, as well as a medical billing section.
PROS:
• Most of what a practice need is included in the system
• There is no need to be concerned with multiple integrations or vendors
CONS:
• Tends to have a higher ‘entry’ cost
• Usually designed for the “middle-of-the-road,” therefore sometimes doesn’t properly address specific needs of a practice
• Sometimes, the practice is left paying for additional customizations to fit their particular needs
SPECIALIZED SOFTWARE:
Specialized medical billing software, on the other hand, is particularly programmed to maintain billing details of tests, procedures, examinations, diagnoses, and treatments conducted on patients. However, many specialized software providers extend their scope to include features like practice management, scheduling, and other administrative and clinical functions (that are generally a part of EHR software systems) by partnering with other specialty software companies—creating a “best-in-class” solution.
PROS:
• Integrating multiple “best-in-class” software packages—each taking a much more focused approach—creates an offering with much more in-depth capabilities
• Usually are more ‘nimble’ in responding to industry and regulatory changes
• More ’scalable’ in supporting the growth of a practice
CONS:
• Most of the time the practice has to deal with multiple vendors
CONCLUSION:
Where “all-in-one” solutions offer a wide breadth of capabilities across the business, they usually also lack focus, depth, and sophistication. “All-in-one” solutions are usually only efficient in one area, with the other areas tend to be ‘compromised’ and not fully developed. Then, when it comes to flexibility, they tend to be slow to adapt to changing practice needs.
Specialized software, however, typically offer a more efficient experience, with each ‘component’ streamlined and designed with a specific purpose in mind. Their focus on limiting the software scope makes them flexible and easy to use.
EZClaim—a leading software package in medical billing and practice management—has made it easier for the medical practice to have the benefit of a “all-inclusive” solution. They have created the best of both worlds by taking on the responsibility of integrating the “best-of-breed” into a harmonized “best-of-class” offering that allows the practice to pick and choose for their specific needs. The seamless integration of partner products and services ensures the practice does not have to give up robustness and flexibility for a simplified “all-in-one” solution, and it further enhances the practice’s workflow.
As a specific example, one of EZClaim’s partners is TriZetto Provider Solutions (TPS), a provider that seamlessly blends claims processing with revenue management and analytics software, so the practice can get paid faster, and more accurately.
Today, the practice can get the benefit of all the power and ease of use of EZClaim’s medical billing software and all the access and security that is needed when dealing with personal records by using TPS—which includes patient access, claims and denials management, patient financials, and advisory services.
The powerful integration between EZClaim and TPS efficiently adds functionality to the practice. Now the practice can gain deeper insight into the claim lifecycle, and take the proper steps to improve the overall health of the practice. The right ‘integrated’ solution makes all the difference!
So, if your practice needs more confident billing, after payments, and more informed decisions, but the power of EZClaim and TPS to work for your practice with the integrated suite of revenue cycle solutions.
In addition to TPS, EZClaim has tightly integrated a variety of of ‘components’ to be able to offer an “all-inclusive” best-in-class solution for a medical practice’s needs: Electronic Health Records (EHR), Clearinghouse, statement and payment services, HIPPA compliance, claims scrubbing, appointment reminders, and inventory management. It has partnered with a variety of providers like QuickEMR, BestNotes, and PracticeFusion [ Click here for an entire list of EZClaim’s partners ].
It is important to note that an “all-in-one” solution does not usually include the Clearinghouse portion that TPS offers. The powerful integration between EZClaim, TPS, and EZClaim’s EMR partners, efficiently adds functionality to ANY practice!
If you are considering the best course of action to meet your practice’s needs, consider using EZClaim by downloading a FREE TRIAL or contact one of their product specialists today to explore all the options for how to best solve your practice’s operational challenges, and grow your business.
For details and features about EZClaim’s medical billing software, visit their website.

Mar 10, 2020 | Health eFilings, Partner
There are many commonly misunderstood aspects and nuances with the MIPS program, particularly in how points are earned. For a healthcare practice, it can be challenging to know exactly what to do to earn points, optimize the score, and protect their Medicare reimbursements. But, at the same time, the stakes have been raised every year and the final ruling of the program is even more complex than it has been in the past, further increasing the stress, burden, and financial risk for a healthcare practice.
The approach a practice takes to report for MIPS will greatly impact the results. Many do not understand or have awareness of, the different reporting methods available to them. Many Providers erroneously still think that a registry is the only reporting option available to them or that they are required to use a registry. Or, they think that their EHR covers their reporting obligation or that an EHR’s reports satisfy the MIPS requirements. These misperceptions and erroneous assumptions are detrimental to the financial interests of any practice.
There is a third reporting methodology that has been established and authorized by CMS, called CEHRT, or Certified EHR Technology (software). The CEHRT methodology assists CMS with their need for more valid data submitted through technology and to refocus Providers from merely using technology towards Providers leveraging technology to improve outcomes. Reporting via a CEHRT using software that has been certified by the ONC is a superior approach because it optimizes the points that could be earned and therefore, maximizes Medicare reimbursements for the practice.
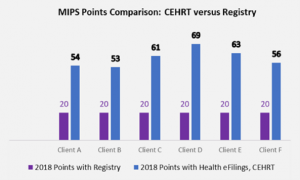
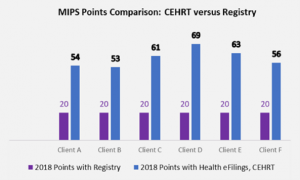
Recently an RCM company CEO approached us at Health eFilings with the decision to use six of her clients to conduct a side-by-side comparison of the registry and Health eFilings (CEHRT) methodologies for reporting. In this manner, she intended to validate for herself whether a CEHRT or registry would generate the greatest ROI for her clients. The results of using Health eFilings’ MIPS Accelerator service, on average earned almost triple the points versus a registry for the same year for the same clients.
“Due to limited understanding and guidance, we weren’t aware of the differences of the reporting methodologies available for my clients. We believed there was greater opportunity, but the current registry methodology we had chosen didn’t demonstrate that for our clients.”
Katy, RCM Company CEO
This side-by-side comparison highlights not only that a CEHRT is a superior method of reporting as Health eFilings was able to leverage technology to facilitate the ease, accuracy, and completeness of tracking and reporting, but it also maximizes a Provider’s MIPS score. Additionally, given the levels of Medicare reimbursements for these practices, the higher score resulted in their earning a positive payment adjustment, which significantly improved their bottom line. And, take note that if the Registry were to perform the reporting for the 2019 reporting period, these practices would not earn enough points to avoid the penalty of negative 7%.
Health eFilings with its proprietary ONC certified software has many advantages over any type of registry:
- Automatically extracts data from any EHR or billing system
- No staff or IT time required to comply
- Benchmarks performance versus peers based on CMS standards
- The proprietary algorithm evaluates 9 million combinations to select the best quality measures to optimize the score
- Earn 10% in bonus points for the Quality category
- eCQM deciles earn more points than registry deciles
- Almost all eCQM’s have a CMS benchmark versus less than 25% of registry measures
- Electronically submits the data to CMS
And, important to note that it’s NOT too late to comply for the 2019 reporting period as Health eFilings is able to support new clients, but time is of the essence. Reach out NOW if you or your client hasn’t reported for 2019—there is NO REASON to accept the 7% revenue hit.
Now EZClaim and Health eFilings want to ensure you can partner with the only complete, end-to-end MIPS compliance solution that saves you significant time and money. To learn more, click the following link: https://healthefilings.com/ezclaim
[ Article was written by Sarah Reiter, Vice President of Strategic Partnerships with Health eFilings ].