Apr 5, 2021 | Medical Billing Software Blog, Revenue, Support and Training, Trizetto Partner Solutions
In the world of healthcare revenue cycle management, there are numerous scenarios that can put a stranglehold on your revenue if you’re not prepared. With the COVID-19 pandemic causing varying degrees of change in inpatient volumes and visits, and telemedicine coming further into play, physicians and their practices are having to quickly navigate the nuances of their financial well-being. A practice may be buttoned up from the time the patient walks in the door, but what happens after the visit will determine when the practice will get paid. This element of the revenue cycle starts with coding. Here are five medical coding challenges that will ruin your bottom line.
1. Coding to the Highest Specificity
Missing data on a claim relative to the patient’s diagnosis and procedure can easily cause a rise in denials once received by the payers, resulting in potentially thousands of dollars in write-offs. Medical coders are responsible for coding patients’ claims to the highest level of specificity, ensuring the appropriate CPT, ICD-10-CM, and HCPCS codes are applied based on the patient’s chart from the day’s services.
COVID-19 and telemedicine are frequently bringing on new codes and code sets, all with different variations and modifiers to make the matter even more complex. Medical coders spend a lot of time researching and learning new codes, but every year – and throughout the year – changes and updates are made. Payers don’t only want to know the diagnosis and the treatment; they want to know the cause as well. The Coronavirus Aid, Relief, and Economic Security Act passed in March of 2020 allows for an additional payment from Medicare of 20 percent for claim billed for inpatient COVID-19 patients, however, it was later indicated that a positive COVID-19 test must be stored in the patient’s medical records in order to be eligible for this payment. Being able to stay on top of codes specific to the patient’s diagnosis at treatment is more difficult than ever before.
2. Upcoding
While code specificity is important, so too is ensuring the claims do not contain codes for exaggerated procedures, or even procedures that were never performed, resulting in reimbursement for these false procedures. This seems logical enough, but upcoding can easily occur as a result of human error, misinterpretation of a physician’s notes, or lack of understanding of how to appropriately assign the thousands of ICD-10-CM codes in existence. To add to the pressure, the Office of the Inspector General issued a plan with objectives to prevent fraud and scams, and remedy misspending of COVID-19 response and recovery funds.
Much like under-coding or not providing enough data on the patient’s visit can create issues, upcoding can be a major contributor to financial loss for a practice. Questionable claims can be denied and sent back for corrections and appeals, but upcoding can have more serious ramifications outside of paper-pushing between coders and payers.
Whether it’s making sure the codes are in accordance with the care provided, understanding the code sets that apply for each procedure, or comprehension of the medical record, refraining from upcoding will help ensure a sturdy and compliant revenue stream.
3. Missing or Incorrect Information
There’s a common theme to coding challenges, and that’s having the sufficient information necessary. This information typically is pulled from a patient’s chart or record of a visit, which is often completed by the attending physician. However, even when a claim is submitted, providing required information relative to the procedure to the payer is critical as well. Situations such as failure to report time-based treatments (such as anesthesia, pain management, or hydration treatments) or reporting a code without proper documentation can result in denials.
Furthermore, information in a patient’s electronic health record may also contain inaccurate information. Keystrokes and other human errors can cause these situations to flare up, and it takes a diligent, thoughtful coder to read between the lines and ensure claims have the appropriate information.
4. Timeliness of Coding
The Medical Group Management Association (MGMA) suggested in their 2018 Setting Practice Standards report that a Primary Care Physician should maintain a claim submission rate of 3.11 days after the date of service, but it is becoming increasingly difficult for practices to sustain anything close to this rate. Constant changes to code sets, an increased focus on submitting claims with sufficient and compliant information, and the requirement to code claims to the highest level of specificity, can easily delay the submission by days or weeks.
Nevertheless, delays in coding and submitting claims can cause major lags in payment and substantial loss in revenue. Insurance payers have statutes of limitations that require claims to be submitted anywhere from 120 to just 60 days after the date of service. Simply put – the more time spent coding the claim, the later it will be submitted, thus increasing the odds that the claim will be denied. Expert coders are aware of this and do everything in their power to get coded claims out the door.
5. Staffing Shortages
However, finding experts well versed in coding claims quickly, accurately and in compliance with the False Claims Act is not always an easy task. As you can imagine, the increasing need for care within the senior population is causing a rise in claim volumes, and trying to find a team of coders who know the ins and outs of complex ICD-10-CM coding can easily cause a bottleneck in the revenue cycle. Health executives expressed their struggles to find talent back in 2015, and some forecasts expect a decline in commercial payments by 2024 to further hamper a C-suite’s ability to manage labor costs. The ramifications of incorrect coding are still a key topic of discussion to this day.
The time has come for practices to begin looking outside of their organization for coding support. How is your practice planning to tackle the coding conundrum? When choosing a partner for your medical coding needs, you need to pick an expert to help your practice stay on target. TriZetto Provider Solutions, a Cognizant Company, has available highly-trained, AAPC & AHIMA certified coders with the experience of getting the details right the first time and understand the importance of coding to the medical practice.
For more information about TriZetto Provider Solutions, a partner of EZClaim, visit their website, contact them, or give them a call at 800.969.3666.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call them today at 877.650.0904.
[ Contribution of the TriZetto Provider Solutions Editorial Team ]
Mar 10, 2021 | BillFlash, Claims, collections, Credit Card Processing, Fullsteam, Medical Billing Software Blog, Revenue
How to Modernize Your Medical Billing Payments Now
It is now very important to modernize medical billing payments capabilities since upwards of 80% of medical services that don’t get paid by insurance, never get paid!
Are you tired of providing medical services and not getting paid? Have you billed patients for their medical visit or co-pay just to find out that the bill showed up in collections? Are you looking for a better way to use modern technology to increase the number of medical claims being paid on time? If you own a medical practice or work in the medical billing industry, then chances are you have answered each question with a hearty “Yes!”
Last month, medical billing industry leaders came together to discuss how medical practices can streamline their payment systems and integrate credit card processing into their billing system. [ Participants: Dan Loch (VP of Sales & Marketing, EZClaim), Tony Peterson (VP of Business Development, BillFlash), and Michael Jones (Payment Services Analyst, FullSteam) all joined host Susan Martinez (Sales Consultant, EZClaim) ].
[ Click Here to LISTEN to the Exclusive Podcast ]
[ Click Here to VIEW the Exclusive Video ]
KEYS That Came Out of the Discussion:
• CHANGING SYSTEMS AND PROCESSES: The practices that are winning in the payment collections game, and seeing the highest percentage of claims paid, are the offices that have updated their systems from the old school and traditional forms of payment collection to the modern, state-of-the-art systems with payment integration. Plain and simple, this means first educating the patient from the moment they walk in the door and streamlining your payments into one medical billing system to prevent human error. [ Click here to LEARN MORE ].
• STREAMLINING CREDIT CARD PROCESSING: Practices often have jumped headlong into credit card processing by using simple systems with variable fees like Square or Stripe. The problem with that is two-fold: First, understanding processing fees, and secondly, avoiding the errors that occur in the steps of processing those purchases over to the billing record. However, now EZClaim’s medical billing software has an integrated payment feature—which streamlines the billing and simplifies the fees. [ Click here to LEARN MORE ].
These are only a few of the very informational topics that were discussed during this podcast. If you are interested in learning how your practice can put these systems in place, increase patient payments, and simplify your billing process in your office, then click here to listen to the podcast and prepare to learn some new, up-to-the-minute ‘insights’ on modern medical billing systems.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call them today at 877.650.0904.

Jan 11, 2021 | Medical Billing Customer Service, Medical Billing Software Blog, Medical Billing Software Customer Service, MIPS Reporting, Revenue
It goes without saying that 2020 will go down in the history books as unprecedented for us at EZClaim. Still, we worked hard to stay positive and navigate the storm by offering resources to you, our clients, the content that matters to you. As an end-of-year bonus, and a ‘kick-off’ for 2021, we reviewed the blogs and social posts you read and reacted to the most and thought we would share them.
So, here are the best blog posts of 2020:
#1: How to Improve Medical Billing Revenues
As a medical billing company, we work hard to understand how we can help our clients increase their revenue and improve their billing process. Those who do this best are experts in the medical billing and coding industry. So, it makes complete sense that your interest peaked on our article concerning improving revenues. Enjoy reviewing our number one article of 2020! [ Click to read the post ].
#2: What Will Be New for E/M Coding in 2021?
Last year brought about a long list of changes to billing and coding, as well as, the medical industry as a whole. From the obvious boom in Telehealth, to the updates in evaluation and management services, those working in the industry were impacted immensely. Based on these shifts in industry and the impact on you, our clients, we thought a look into what was coming in 2021 would be useful—and so did you. You read, reacted, and shared the value of this content with others. Now we are sending you a reminder that this was our number two article for the year. [ Click to read the post ].
#3: Collecting Payments from Patients. Find Out How.
No matter how chaotic things get, there is still a practical side of our industry that needs to be addressed. That is why we worked to keep the focus on the basics, speaking about the ‘bread and butter’ of our industry, collections. In this practical article, we focused on the keys to educating the patient and how doing so will help keep you ahead of the collection as a whole. [ Click to read the post ].
#4: Reports – Nuisance or Necessity?
At the end of the day, you want to go home and no one wants to be stuck in the office doing double-duty on reports. You know as well as we, that getting reports done correctly the first time is key to reducing stress and going home happy. That is why we distilled some of the keys in running reports that would make your life more straightforward. The fourth article on our list will do just that by helping you make sure the dates, details, and destination of your reports are in the right place. [ Click to read the post ].
#5: Why Do I Have A Balance? – Patient Payments
Saving the best for last, especially as we approach tax season, we come in with our final of our best of 2020 by talking about balances. Every practice ends up spending those final hours of the year figuring out where those dollars and cents went. In this article, we gave you tips on deductibles, co-pays, and max out-of-pocket that helps your bottom line. Closing out 2020, don’t miss a few keys to help you balance the books. [ Click to read the post ].
These are EZClaim’s best blog posts of 2020, but these were not the only blog posts we did. So, if you would like to explore the other blog posts we did, click here for our blog page.
————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail support, or call a sales representative today at 877.650.0904.
Nov 10, 2020 | Medical Billing Software Blog, Partner, Revenue, Support and Training, Waystar
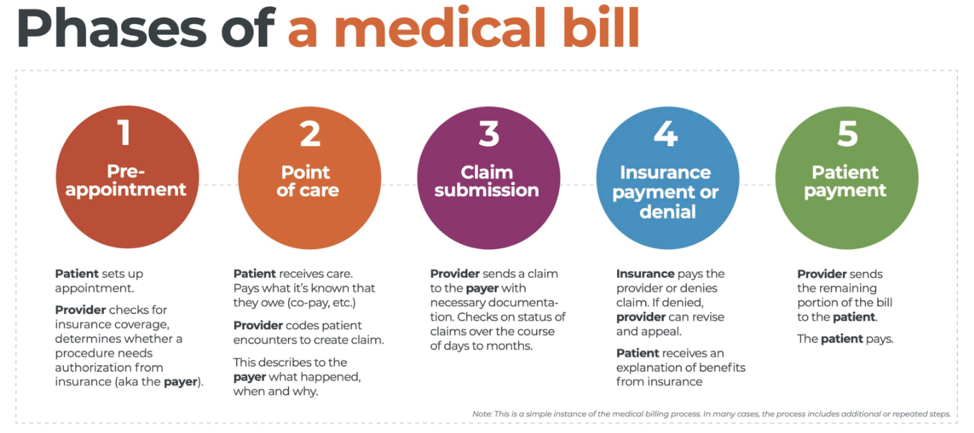
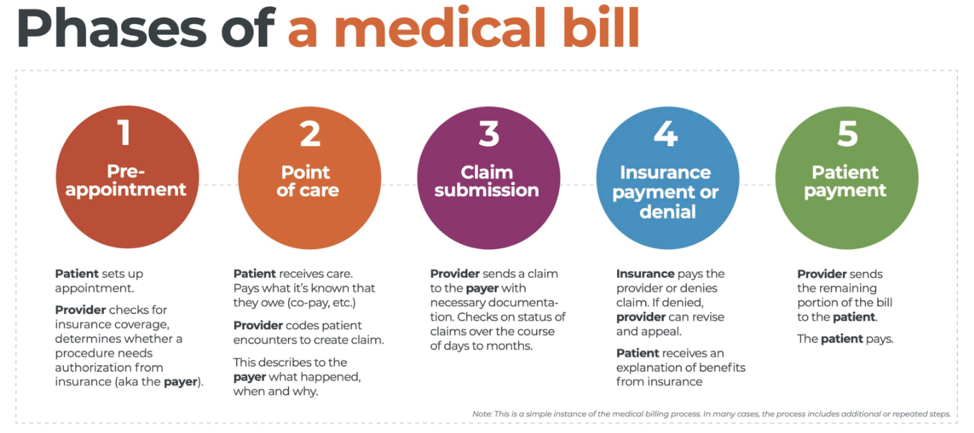
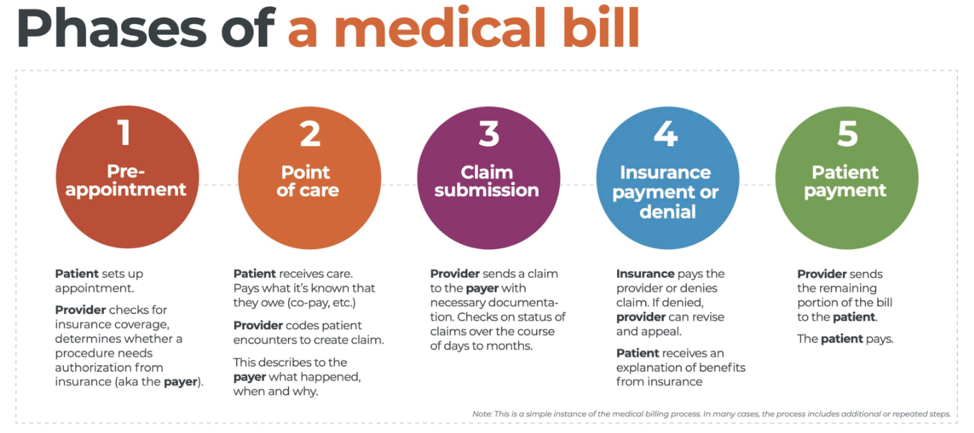 There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.
There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.
With high deductible health plans on the rise, the recent explosion of telehealth appointments due to COVID-19, and many other factors in play, it’s more important than ever for everyone to understand the life cycle of a medical bill, and how the process works. The healthcare revenue cycle is relevant not only to those who work in healthcare, but to the patient, too.
The revenue cycle is the series of processes around healthcare payments—from the time a patient makes an appointment to the time a provider is paid—and everything in between. One way to think of it is in terms of the life cycle of a medical bill. Although there are many ways this process can play out, this post will lay out a common example below:
1. Pre-appointment
For most general care, the first stage of the revenue cycle begins when a patient contacts a provider to set up their appointment. Generally this is when relevant patient information will begin to be collected for the eventual bill, referred to on the financial side of healthcare as a claim.
At this point a provider will determine whether the appointment and procedure will need prior authorization from an insurance company (referred to as the payer). Also, the electronic health record (EHR) used to help generate the claim is created, and will begin to accumulate further detail as the provider sends an eligibility inquiry to check into the patient’s insurance coverage.
2. Point of care
The next step in the process begins when the patient arrives for their appointment. This could include when a patient arrives for an initial consultation, an outpatient procedure, or for a follow-up exam. This could also include a Telehealth appointment.
At any of these events, the provider may charge an up-front cost. One example of this is a co-pay, which is the set amount patients pay after their deductible (if they are insured), however, there are other kinds of payments that fall into this category, too.
3. Claim submission
After the point of care, the provider completes and submits a claim with the appropriate codes to the payer. In order to accomplish that, billing staff must collect all necessary documentation and attach it to the claim. After submitting the claim to the payer, the provider’s team will monitor whether a claim has been been accepted, rejected, or denied.
[ Note: Medical coding refers to the clerical process of translating steps in the patient experience with reference numbers. The codes are normally based on medical documentation, such as a doctor’s notes or laboratory results. These explain to a payer how a patient was diagnosed and treated, and why. This information helps the payer decide how much of an encounter is covered under any given insurance plan, and therefore how much the payer will pay. ]
4. Insurance payment or denial
Once the payer receives the claim, they ensure it contains complete information and agrees with provider and patient records. If there is an error, the claim will be rejected outright and the provider will have to submit a corrected claim.
The payer then begins the review process, referred to as adjudication. Payers evaluate claims for accurate coding and documentation, medical necessity, appropriate authorization, and more. Through this process, the payer decides their financial obligation. Any factor could cause the payer to deny the claim.
If the claim is approved, the payer submits payment to the provider with information explaining details of their decision. If the claim is denied, the provider will need to determine if the original needs to be corrected, or if it makes more sense to appeal the payer’s decision.
Following adjudication, the payer will send an explanation of benefits (EOB) to the patient. This EOB will provide a breakdown of how the patient’s coverage matched up to the charges attached to their care. It is not a billing statement, but it does show what the provider charged the payer, what portion insurance covers, and how much the patient is responsible for.
5. Patient payment
The next phase occurs when the provider sends the patient a statement for their portion of financial responsibility. This stage occurs once the provider and payer have agreed on the details of the claim, what has been paid, and what is still owed.
The last step occurs when a patient pays the balance that they owe the provider for their care. Depending on the amount, the patient may be able pay it all at once, or they might need to work with the provider on a payment plan.
The above example represents one way the lie cycle of a medical bill can play out. Some of the ‘phases’ are often repeated. Because of the complexity of healthcare payments and the parties involved, there is not always a ‘straight line’ from patient care to complete payment. That’s why we call it the revenue cycle, and there are companies that provide systems for its management.
One of EZClaim’s partners, Waystar, aims to simplify and unify healthcare payments. Their technology automates many parts of the billing process laid out above, so it takes less time and energy for providers and their teams, and is more transparent for patients (Click here to learn more about how Waystar automates manual tasks and streamlines workflows.) When the revenue cycle is operating at its most efficient, providers can focus their resources on improving patient care—and that’s a better way forward for everyone!
For more information of how Waystar works together with EZClaim, click here.
[ Article and image provided by Waystar ]
———————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support, and can help improve medical billing revenues. To learn more, visit their website, e-mail them at sales@ezclaim.com, or call a representative today at 877.650.0904.

Nov 10, 2020 | Alpha II, BillFlash, Claims, collections, Denied Claims, EZClaim Premier, HIPAA, Medical Billing Software Blog, Revenue, Support and Training
It IS POSSIBLE to improve medical billing revenues, and here are a few ways to do just that.
Healthcare practitioners, whether established or just starting out, have many overwhelming tasks: Managing a practice; Seeing patients; Working to staying up-to-date on administrative tasks; The whole host of compliance at the federal, state, and local level; and Overseeing the billing.
One of these that can lead to loss of revenue is not properly managing the medical billing, which can also lead to HIPAA fines and rejected claims. However, there is a solution: a medical billing system that balances the budget and optimizes revenues of medical practice.
EZClaim, an expert in the medical billing software market since 1997, provides a solution that improves the efficiency of an office’s billing process in many ways. The following are the primary reasons.
Reduce Coding Errors
Medical procedures become codes, codes become claims, and claims become revenue. Any error in this process can make claims to be denied, your workload can be increased, and revenue can be lost. To help in avoiding errors, it is essential to use billing software that offers the easiest implementation and access to descriptive diagnosis and treatment codes. EZClaim’s medical billing solution offers ease-of-use in coding, billing, and strong partnerships with Clearinghouses which act as an additional ‘safety net’ for catching errors.
Administrative Support
Most medical practices are a small team of people tackling a wide range of tasks, so when one cannot understand the function of the billing software, accessing reliable support is very important. EZClaim prides itself on having dedicated support experts available, and that was how the company was established. Founder and President Al Nagy has said, since day one, “We are a support company that happens to sell medical billing software.”
Maintain Industry Compliance
It is important to recognize that industry compliance and a practice’s revenue go hand-in-hand. Filing and batching inaccurate and non-HIPAA compliant claims can often be traced back to an outdated healthcare revenue management system. Conquering these tasks requires a focus on multiple fronts: A properly trained billing team, clear office procedures, patient payment policies, and a reliable medical billing company. These are all ways to help buttress against non-compliance and rejected claims.
Streamline Workflow
Recently, a study was done that showed almost 80% of medical bills contain errors. These incorrect medical claims often end up as lost revenue originally, not to mention the additional cost of resubmissions and collections. One of the best ways to resolve this problem for your practice is to make use of both well-trained, experienced billers and coders, combined with a competent medical billing solution that aids in catching these errors. EZClaim software features a library of standard validation, the ability to add custom validation, and integrates with Alpha II for full claim scrubbing.
Follow up
Errors will and do occur, so establishing a system for follow-up on all denials will close the loop and protect against lost revenue. Being consistent with the follow-up process, and having a medical billing solution that tracks these things will help close that gap.
Collections
Finally, probably the most important aspect that optimizes a practice’s revenue is to get paid. Portals and payment collection systems definitely help with this, but having collections integrated into the medical billing system is, of course, the best. EZClaim has pain-free payment processing integrated into their solution, called EZClaimPay. It solves all the problems associated with payment processing: Bank deposits, reconciliation, statements, changing fees, and ‘finger-pointing’ when there is a problem. EZClaimPay’s robust platform will greatly increase a practice’s collections success, and improve their revenue.
———————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support, and can help improve medical billing revenues. To learn more, visit their website, e-mail them at sales@ezclaim.com, or call a representative today at 877.650.0904.
[ Photo credit: Studioarz ]


Oct 13, 2020 | BillFlash, Revenue, Webinar
Feeling overwhelmed by the complexity of the revenue cycle management process? This webinar will help you identify the most important measures affecting practice revenue, will explain how to make improvements to improve cash flow, as well as how to save your staff time.
PRESENTED BY: Stephanie Cremeans, CPC, CPMA, CPPM, Founder of RCM Insight
Wednesday, November 4th at 11 am MT/1 pm ET
You Will Learn The Following:
- Creating scorecards to eliminate issues that are preventing payments
- Identifying and improving processes that improve revenue
- Organizing staff to monitor and improve the financial process
- Avoiding the pitfalls of uncompensated care
- Teaching & training to get results
______________________
About Stephanie Cremeans:
Stephanie has served in various roles in the medical billing and coding field including Revenue Cycle Manager, Consultant, Auditor, Biller and Coder. Stephanie has a passion for educating providers, coders, and billers on how to maximize revenue through proper documentation and effective workflows. She has worked with several specialties including family medicine, cardiology, physiatry, urgent care, GI, pediatrics, OB/GYN, and behavioral health.
Click here to register for the BillFlash Webinar, “Simple Tips to Improve Your Practice’s Cash Flow Process“