May 11, 2021 | Features, Medical Billing Software Blog
Can you add up the number of hours your billing team spent during any given week or month waiting on-hold with insurance companies to get patient billing information? Does your staff invest hours of their valuable time seeking out the smallest of details to get paid? Are you aware that integrated eligibility, through EZClaim’s medical billing software, can reduce that time on-hold to a fraction of the total?
It is estimated that the average biller can spend up to 2-hours on-hold just to get an insurance company on the phone. Add to that an average of 10 – 15 minutes to talk through a patient and most companies will only address one or two patients at a time. To add to it often there are multiple insurance companies to call. As you can tell you quickly have a considerable amount of time lost making phone calls. Instead of spending hours on the phone with insurance companies, make best use of your staff’s time by checking to see if you have the integrated eligibility feature in your billing software.
Getting started is as easy as getting set up with a clearinghouse (EZClaim clearinghouse partners). Once you are signed up with a clearinghouse for the electronic claim submission program, they will have an integrated eligibility feature that is integrated into EZClaim. Once you sign up with this feature, you can send a batch request of 50 patients at one time and if needed, send multiple requests in a day. Do this by selecting an active patient list collectively or send them individually in smaller amounts. Either way the time savings will be exponential.
Eligibility response reports often come back within seconds making the process nearly real-time. When a response comes back you have the real-time eligibility information. You will get details on if they are covered or not, their active dates, deductibles, co-insurances, co-pays, and what amounts they are subject to and what will be deducted. With EZClaim eligibility integration built in you save valuable time. To learn more contact EZClaim’s website, email, or call 877.650.0904.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.

Feb 9, 2021 | Claims, Electronic Billing, Features, Medical Billing Customer Service, Medical Billing Software Blog
Are you working in the medical billing industry as a biller or an owner of a billing company? If so, the KEY medical billing insights and best practices that came out of our interview with Maura Jansen (VP of Operations) and Jennifer Withington (Director of Revenue) at Missing Piece Billing & Consulting Solutions will be VERY VALUABLE for you to consider.
Jennifer, an expert in understanding the problem-solving techniques and the investigative nature of medical billing, offers insights that both educate and inspire. Maura, an executive member of the billing community, also added an important perspective about EZClaim’s medical billing software. The following are some highlights from our interview.
EZCLAIM: When did you get into the industry?
JENNIFER: “I worked in group homes for the waiver side of group aid and then I went to Missing Piece. Missing Piece primarily deals with ABA providers and provides early intervention rendered to children. For me, the move from waivers with adults to professional billing, indirectly assisting children, was attractive and I took to the billing side of things.”
EZCLAIM: What does that mean when you say you took to the billing side of things?
JENNIFER: “Insurance doesn’t make a lot of sense when you first start. So, I took to the investigative side of making sense of medical billing claims. Figuring out what the payer’s rules are, reading their manuals, and figuring out the technical jargon with the purpose of preventing claim denials was attractive. I liked the puzzle of it.”
EZCLAIM: Are there things that you value in your work that offer meaning to what you do?
JENNIFER: “It’s really when I know that if I do not intercede with the insurance company and get this paid the patient is going to be responsible for the balance. So, to help, I have taken things to the department of insurance, or I have gone ahead and filed that third letter of appeal and really taken the time to research it. Because I don’t want a parent who is already struggling with having a child with more needs than maybe the other children would have, I don’t want them struggling with a $25,000 bill. ABA is extremely expensive because it works. And so, if insurance doesn’t pay it then the only other funder is the parent. And my goal is that parents should not have to pay any more than they absolutely have to.”
EZCLAIM: What are some of the strengths that make you good at what you do?
JENNIFER: “I am a good problem solver. I am good at taking a large problem and breaking it into smaller problems and knocking each one down until I solve the bigger issue. At the end of the day, that’s really what accounts receivable is.”
EZCLAIM: What would be an example of your problem solving on a day-to-day basis?
JENNIFER: “So you always start with the denial and then you have to work back to the billing. For example, if I have a claim denied for services rendered from an out-of-network service provider, but we know we are in-network then my first problem is, are we actually in-network? Then, you go onto the next link which is did the payer recognize you as in-network? It becomes like a decision tree, if you get a ‘yes’ then you are probably done, and you get the claim processed. If it is ‘no’, then you have to start digging with the payers contacting reps, make calls, and supply them with documents to get down to why they don’t have your provider listed within the network. Once you solve that problem, then the claim should be able to be processed. It is either going to pay or deny. Then depending on which one it is, you apply the same technique.”
EZCLAIM: What would you offer someone who is considering entering the field?
JENNIFER: “You should be good at processing and reading information because to get a claim paid you to have to know the rules of engagement. You need to be familiar with how to read a contract, how to read technical information about billing, and have to have a glossary of information about what you are billing. Those are the building blocks to get to know what you are doing.”
EZCLAIM: You work with EZClaim’s medical billing software platform, what role does their software providers and how does that impact your work?
JENNIFER: “EZClaim really serves to eliminate these denials before they happen, which is the ultimate goal of any accounts receivable or billing. EZClaim has edits that we use. It alerts us if the system thinks the claim is a duplicate, for example. It also helps in the set-up of the claim. We load all the fee schedules in EZClaim’s procedure code library and that lets us monitor the charge rate, make sure all the points of billing are on the claim (i.e. correct code, modifier, and charge). They also make sure that the authorization is appended to the claim. And then after we have actually done the work of getting a claim in the system, we use EZClaim reports to audit our own billing. So, we use the EZClaim service report. It makes it easier for us and our providers to see what has been billed and make sure that the billing is correct.”
EZCLAIM: If you were going to share something with your colleagues in the field, what would you share about the software that makes your life easier?
JENNIFER: “Number one, it is not the software itself, it’s the EZClaim staff. Their customer service is far beyond what a normal billing software company provides. If I have a problem, or if I have a report, or if I have a data point that isn’t in any report, they are available and they are there for me. And if they don’t have a solution for the problem, they will provide me with a workaround. So, that is very valuable. That is why Missing Piece works so well with EZClaim because customer service is number one for us, too. They don’t just want to answer your question, they want to help you understand your question.”
“The other thing that I find valuable is that their reporting modules are just a lot more robust than the other billing software companies that I have dealt with.”
EZCLAIM: Maura, do you have any thoughts from an administrative level that you can offer on EZClaim?
MAURA: “Well, when we hire a new person we know that, even if this person has very little experience in the healthcare field, it’s going to be a quick and easy process for them to learn EZClaim… EZClaim has also made it kind of a joy to work with. We really value them as a partner. We love the service they provide, and we value them as a platform.”
ABOUT EZCLAIM:
EZClaim can also help you with medical billing insights since it is a medical billing and scheduling software company. It provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.
Jun 10, 2020 | Features, Medical Billing Software Blog
Whether you are an experienced EZClaim user looking to learn a new trick or just starting out with the software, “Find Grids” simplifies medical billing within the EZClaim software.
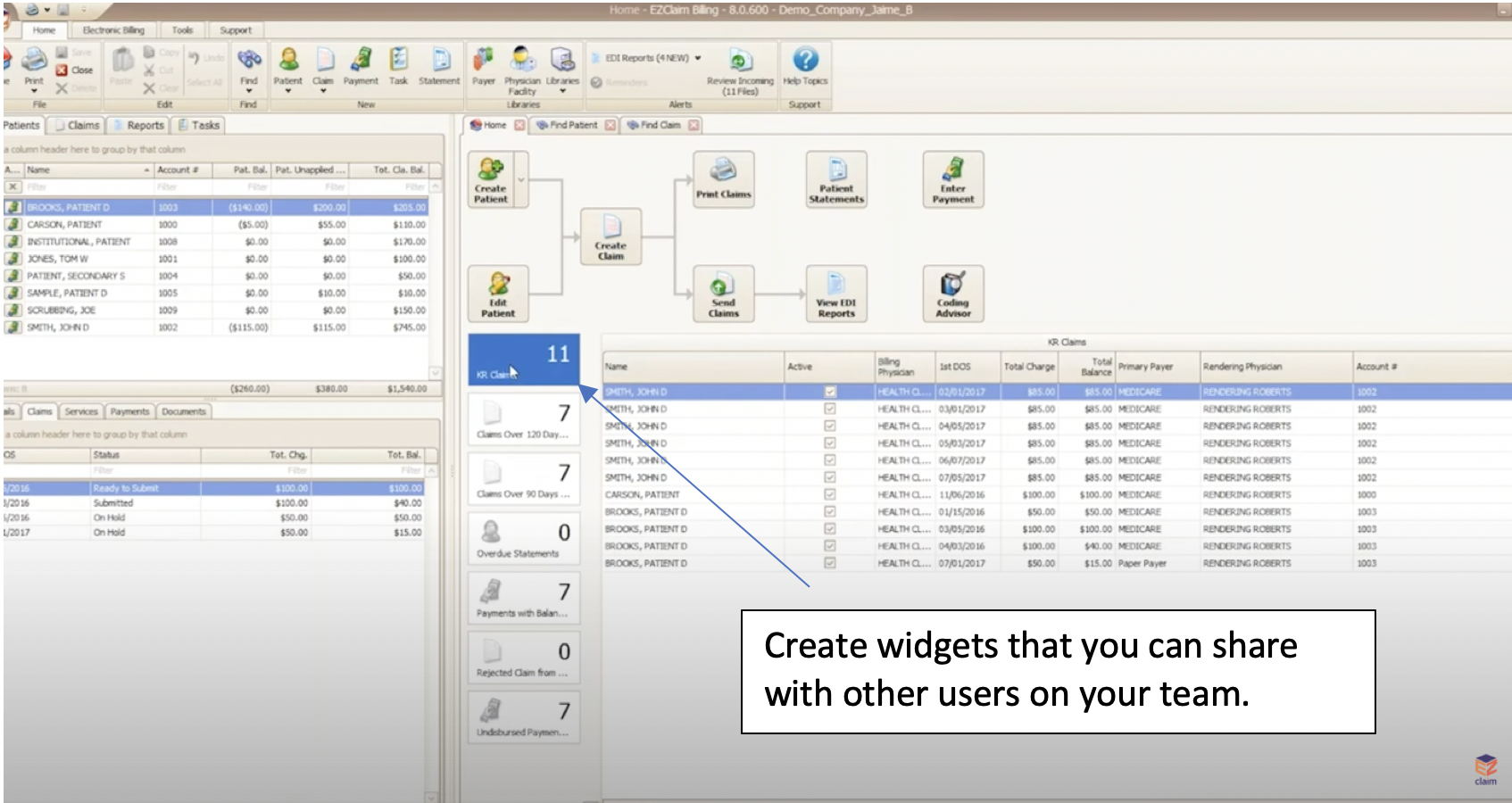
For the average biller, customizing grids is as important as adjusting your mirrors to face in the proper direction before driving your car. At a basic level, grids allow you to sort, filter, and customize your workflow and search needs. However, there is more flexibility available with grouping panels, flexible filtering rows, custom columns, and the ability to create and share widgets within the software—all of which will simplify your billing. (To learn more details, view the “Working with Grids” tutorial below).
CLICK FOR VIDEO: https://www.youtube.com/embed/ikUIM2AVURQ
The grids feature in EZClaim is a very powerful tool since the grids are highly customizable (they function like a spreadsheet). At the click of a button—or the stroke of a key—you can search for data and align your columns in your find claims field. If sorting to a specific set of claims is important to you, a simple click organizes your data to be queried for rendering. Sorting data has never been easier!
To simplify your workload even further, you can create an “established” find grid (i.e. find patient grids, find claim grids, find disbursement grids, etc.). You then can make bulk changes to the status of each claim without dealing with individual touches. Then, once you have created the filtered columns, you can go deeper and create reports that show you exactly what you want by using the filter editor. This is just one more way that EZClaim makes billing simpler and quicker. “Find grids” simplifies medical billing for all who use EZclaim’s software.
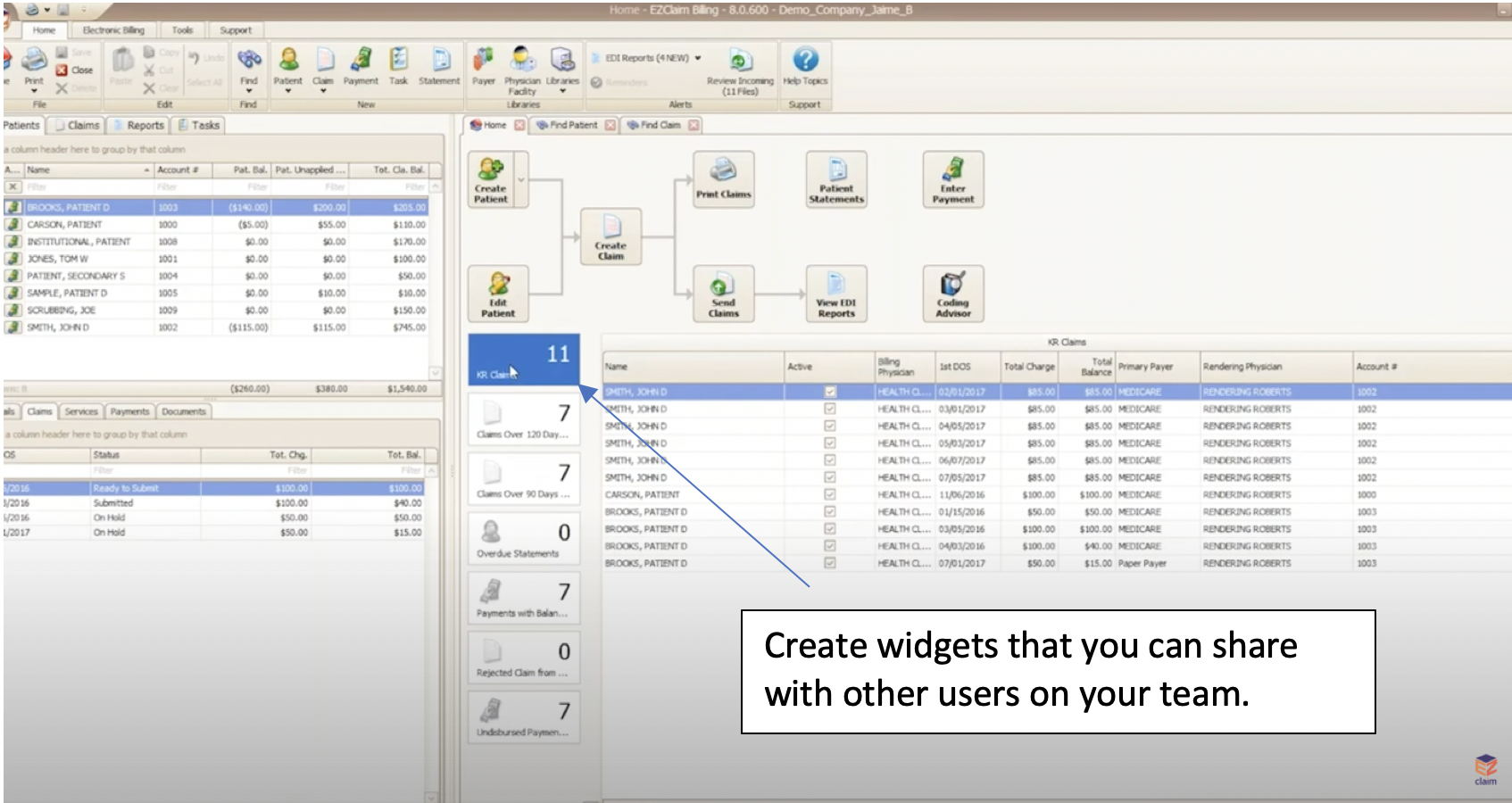 So, here’s a few questions to ask yourself. Is it important for you to customize your grids so that you can find what you need when you’re looking for it? Would you find it helpful to have auto-filters in place and be able to populate your search at the click of a button? Would it be helpful to be able to create a “widget” that you can share with your team?
So, here’s a few questions to ask yourself. Is it important for you to customize your grids so that you can find what you need when you’re looking for it? Would you find it helpful to have auto-filters in place and be able to populate your search at the click of a button? Would it be helpful to be able to create a “widget” that you can share with your team?
Well, if you answered “Yes” to any or all of the above questions, then our tutorial on “Find Grids” (click here to view) will guide you through, step-by-step, the most efficient use of the feature. In addition to that, you can also reach out to our customer service team for more details.
If you are new to medical billing, EZClaim can help with your evaluation. You can either schedule a one-on-one consultation with our sales team, view a recorded demo, or download a FREE 30-day trial right now.
For detailed product features or general information about EZClaim, visit our website at ezclaim.com/