Oct 12, 2020 | Partner, Trizetto Partner Solutions, Webinar
Reserve your place for a webinar that will inform you on how to increase your revenue with a proper medical billing verification strategy.
With increased patient financial responsibility, it’s extremely important to proactively check your patients’ benefits coverage and provide payment estimates to avoid any unexpected costs. By enhancing your medical billing verification strategy and providing patient financial transparency upfront, it increases the likelihood that you’ll rake in more revenue this season.
Join EZClaim and TriZetto Provider Solutions, a Cognizant Company, for a webinar on Thursday, October 29, 2020 at 1 p.m. ET, to discover strategies your practice can catch falling revenue through seamless integration and automation.
During This Webinar We Will Discuss:
• Patient Responsibility Estimation: Quickly obtain patient financial estimates at the point of service to help increase patient revenue, decrease billing costs, and improve patient satisfaction through price transparency.
• Integrated Eligibility: Connect to payers through a single application to get the most up-to-date information on patient coverage, co-pays, deductibles, and more. Proactively verify patient eligibility, for up to 50 patients at a time directly from your EZClaim Premier program.
• Insurance Eligibility Discovery: Submit a real-time eligibility request using minimal data and identify a patient’s insurance carrier in a matter of seconds. Maintain groups of your common payers and easily locate active patients and full eligibility benefits on our website.
RESERVE YOUR PLACE NOW!
ABOUT THE PRESENTERS:
EZCLAIM: EZClaim is a medical billing and scheduling software company that provides best-in-class customer service and support. To learn more, e-mail them at sales@ezclaim.com or call a representative today at 877.650.0904.
TRIZETTO: TriZetto combines innovative, proven products with an exacting commitment to serving our customers, in order to provide you with the tools you need to effectively manage your reimbursement cycle.

Oct 12, 2020 | Electronic Billing, Features, Medical Billing Software Blog
EZClaim Launches EZClaimPay, a new feature in its medical billing software that makes credit card processing painless!
EZClaim, a company with the mission of elevating its clients to stay in front of the ever-changing landscape of medical billing, announced today the launch of its credit card processing feature and service called, EZClaimPay.
EZClaim released the product in August 2020 as a solution to the ever-changing landscape of payment reconciliation. It was cited by customers as a timely response to a ‘pain point’—credit card payment processing—another example of EZClaim’s devotion to their mission.
Dan Loch, VP of Marketing commented that “EZClaim’s goal continues to be making life easier for medical billers at practices and billing firms. EZClaimPay is just one more feature within our mission of living up to that goal.” This feature will help companies get in front of the changes in medical transparency that are coming soon.
EZClaimPay provides for consolidated reconciliation (Payment reports; Chargeback management; and Reconciliation reports) and a single point of contact for support (Hardware; Software; and Payments).
EZClaim has developed a robust payments platform—tightly integrated with their software and support—to make accepting credit cards for payment PAINLESS! EZClaimPay makes software and payments better together.
For more details about EZClaimPay, view this web page: https://ezclaim.com/ezclaimpay/
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides best-in-class customer service and support. To learn more, e-mail them at sales@ezclaim.com or call a representative today at 877.650.0904.
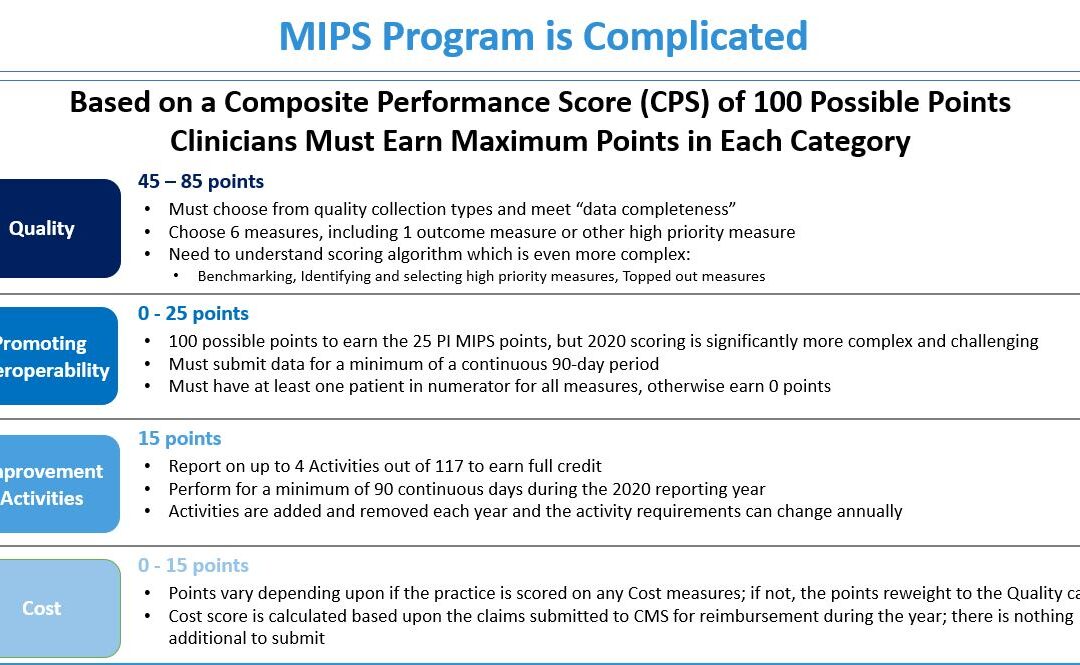
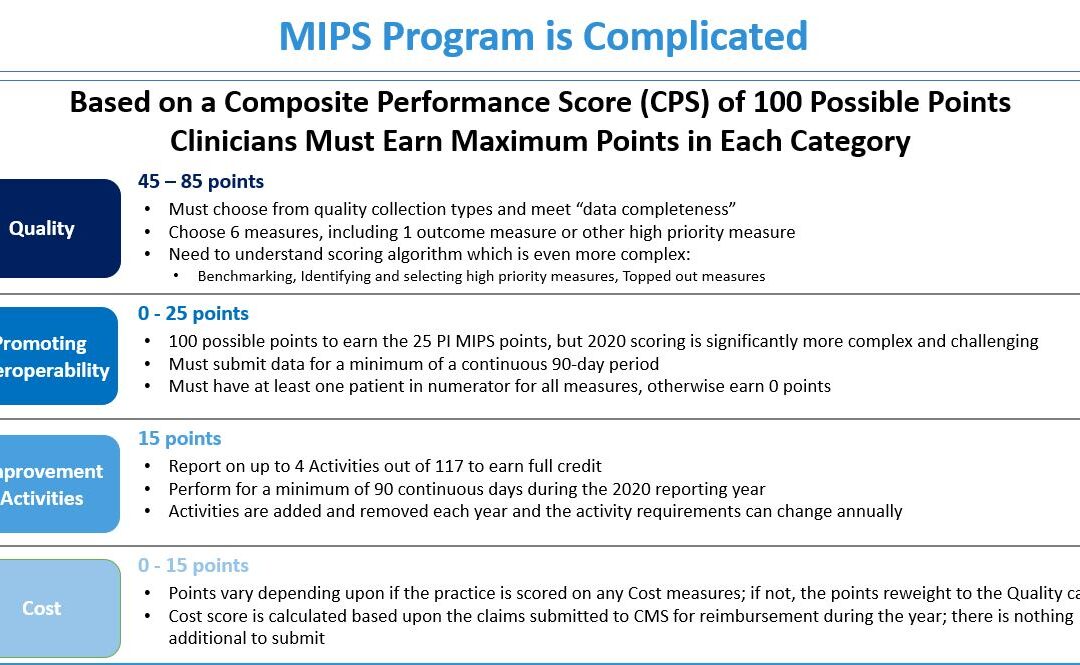
Jul 14, 2020 | Health eFilings, MIPS Reporting, Partner, Revenue
The 2020 MIPS reporting is already half done, and given that MIPS (Merit-based Incentive Payment System) is a points-based program, the goal is to earn as many points as possible to avoid this year’s 9% penalty and potentially even earn a positive payment adjustment. However, earning the 45 points necessary to avoid the penalty for the 2020 reporting period will be no easy feat. With over half of the reporting period already behind us, it is imperative you ACT NOW so you don’t find yourself in a position later in the year that you can’t recover from in terms of earning points.
With all the complexities and nuances of the program, it’s challenging to know what you can do to impact your score. Here are three critical actions to take right now so that you will still optimize your ability to earn points for the 2020 reporting period:
1. Focus on the Quality Category
There are various points available within each of the categories and the Quality Category has the most points associated with it. Based on a number of factors, the category is worth anywhere from 45 to 85 points. This is a critical category to be focused on throughout the year, so now is the time to ensure that you are tracking all relevant data so that it can be properly reported on within your submission.
2. Understand the Timeframe Requirements
Two of these categories, Promoting Interoperability and Improvement Activities, have timeframe requirements where you must perform for a minimum of 90 continuous days. These are not easy categories in which to be successful and so if you wait too long in the year you will find it impossible to put the right actions in place in order to complete the activities necessary to earn any of the points in these categories.
3. Choose the Right Reporting Methodology
Not all reporting methodologies are the same and the reporting methodology you select has a significant impact on the points you could earn. Additionally, there is strategic maneuvering that can be done throughout the reporting period with exemptions and reweighting of points that can set you up to optimize your performance and your score. Therefore, you must select a reporting partner that will help you earn the most points available and leverages technology to facilitate the ease, accuracy, and completeness of tracking and reporting to maximize your score. Reporting via a CEHRT, like Health eFilings, is the best approach because it optimizes the points that could be earned and therefore, maximizes Medicare reimbursements.
Health eFilings is a certified EHR technology (CEHRT) and the national leader in automated MIPS reporting. Their cloud-based ONC-certified software fully automates the reporting process. Because Health eFilings’ service is an end-to-end electronic solution that doesn’t require any IT resources, administrative support, or workflow changes from you, the practice will save significant time while maximizing its financial upside.
To learn more about how to properly perform your 2020 MIPS reporting, contact EZClaim’s partner, Health eFilings, so they can help before it’s too late!
For details and features about EZClaim’s medical billing software, or general information about the company, visit their website.
[ Written by Sarah Reiter, SVP Strategic Partnerships, Health eFilings ]
Jun 10, 2020 | Alpha II, Medical Billing Software Blog, Partner, Revenue, Webinar
Concerned about the claims process during COVID-19? Well, Alpha II remains on the forefront of the coding and billing changes during the COVID-19 public health emergency (PHE). They understand this is a confusing time for providers, practices, and hospitals.
Now more than ever, practitioners are relying on the revenue brought in by accurate claim submission. So, if you would like more up-to-date details, join us for our Bring Revenue Integrity to the Claims Process During COVID-19 webinar on June 16th at 1 p.m. ET, and learn how to recover revenue based on the waivers allowed under the PHE. Click here to register for the webinar.
We have also compiled a comprehensive COVID-19 billing and coding FAQ document of questions received during our highly-attended webinar series. Click here to download the resource.
As guidelines for coding and billing of COVID-19 services are revised regularly, Alpha II is implementing these critical changes to regulations and coding guidance—almost immediately.
Alpha II empowers precision across the revenue cycle process so you can experience reduced cost, improved cash flow, and increased revenue. Through its software-as-a-service (SaaS) solutions, Alpha II supports coding, compliance, claims editing, value-based quality reporting, and revenue analysis.
For more details about how Alpha II’s solutions can keep your coding, billing, and editing current, view our website or fill out our contact form to ask us a specific question.
Alpha II is a preferred partner of EZClaim, and their software is integrated into our medical billing software. For detailed product features or general information about EZClaim, visit our website at ezclaim.com/

May 12, 2020 | Medical Billing Software Blog, Partner, Trizetto Partner Solutions
If you are a member of the MEDICAL BILLING COMMUNITY, the norms of the day-to-day have changed. With the recent COVID-19 pandemic and the ‘stay-at-home’ order, you may find yourself with either more time on your hands and/or an increase of claims with new patients. During this time, we want to offer you a couple of suggestions so that you can make the best use of the additional time you have, and also help you improve your billing processes.
The first thing to consider is to review your Accounts Receivable (AR)—to collect payments due you to INCREASE YOUR INCOME. According to the American Medical Association (AMA), claim denial rates range between 0.5% and up to 3% or more, and that 90% of claim denials are preventable. Some of the most common claim denial reasons can be rectified by correcting claim management workflows, including claim submission and patient registration procedures. The following are a few of the most common oversights for claim denial.
- Use EZClaim software to check automatically for missing information, including absent or incorrect patient demographic information and technical errors
- Make sure you do not have duplicate claim submissions
- Check that claims do not have services previously adjudicated
- Review for claims with services not covered by the payer
- Make sure the time limit for claim submission has not expired
Secondly, revisit and resubmit open claims. Surprisingly, 31% of providers still use a manual process to resubmit. Our partner, TriZetto Provider Solutions (TPS), has an Advanced Reimbursement Manager Pro (ARM) that has two great tools that can improve your ability to tackle collecting and repaying underpaid and overpaid accounts. Below are some key features that can be automated by their software, and will help to improve your billing processes:
- Identify common errors and payer trends
- Analyze contract performance
- Customize and assign work into queues
- Quickly access information from interactive dashboards
- Automate the appeal process
Thirdly, know that EZClaim and our partner TPS have worked together to bring you the most powerful medical billing software tools to solve claim denials. Our partnership not only simplifies the billing process but also helps resolve denied claims in an efficient way. In addition to that, our customer support team is available to help you learn best practices with these tools, and support you however you need it.
Finally, if you are frustrated with your current medical billing solution, investigate how EZclaim’s medical billing solution may work for you. You can either schedule a one-on-one consultation with our sales team or download a FREE TRIAL to check it out the software yourself. For additional information right now, contact EZclaim’s sales team at 877.650.0904 or send an e-mail to sales@ezclaim.com.