Mar 10, 2021 | BillFlash, Claims, collections, Credit Card Processing, Fullsteam, Medical Billing Software Blog, Revenue
How to Modernize Your Medical Billing Payments Now
It is now very important to modernize medical billing payments capabilities since upwards of 80% of medical services that don’t get paid by insurance, never get paid!
Are you tired of providing medical services and not getting paid? Have you billed patients for their medical visit or co-pay just to find out that the bill showed up in collections? Are you looking for a better way to use modern technology to increase the number of medical claims being paid on time? If you own a medical practice or work in the medical billing industry, then chances are you have answered each question with a hearty “Yes!”
Last month, medical billing industry leaders came together to discuss how medical practices can streamline their payment systems and integrate credit card processing into their billing system. [ Participants: Dan Loch (VP of Sales & Marketing, EZClaim), Tony Peterson (VP of Business Development, BillFlash), and Michael Jones (Payment Services Analyst, FullSteam) all joined host Susan Martinez (Sales Consultant, EZClaim) ].
[ Click Here to LISTEN to the Exclusive Podcast ]
[ Click Here to VIEW the Exclusive Video ]
KEYS That Came Out of the Discussion:
• CHANGING SYSTEMS AND PROCESSES: The practices that are winning in the payment collections game, and seeing the highest percentage of claims paid, are the offices that have updated their systems from the old school and traditional forms of payment collection to the modern, state-of-the-art systems with payment integration. Plain and simple, this means first educating the patient from the moment they walk in the door and streamlining your payments into one medical billing system to prevent human error. [ Click here to LEARN MORE ].
• STREAMLINING CREDIT CARD PROCESSING: Practices often have jumped headlong into credit card processing by using simple systems with variable fees like Square or Stripe. The problem with that is two-fold: First, understanding processing fees, and secondly, avoiding the errors that occur in the steps of processing those purchases over to the billing record. However, now EZClaim’s medical billing software has an integrated payment feature—which streamlines the billing and simplifies the fees. [ Click here to LEARN MORE ].
These are only a few of the very informational topics that were discussed during this podcast. If you are interested in learning how your practice can put these systems in place, increase patient payments, and simplify your billing process in your office, then click here to listen to the podcast and prepare to learn some new, up-to-the-minute ‘insights’ on modern medical billing systems.
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call them today at 877.650.0904.

Feb 9, 2021 | Medical Billing Software Blog, Partner, Trizetto Partner Solutions
The COVID-19 pandemic has put a spotlight on the need for mental health resources as illness, job losses, and isolation continues to create unprecedented stress levels. According to recent surveys conducted by the Larry A. Green Center, more than half of clinicians reported declining health among patients due to closed facilities and delayed care, and more than one-third noted that patients with chronic conditions were in noticeably worse health as a result. Even more striking, over 85 percent reported a decline in inpatient mental health with 31 percent seeing a rise in addiction.
With mental health access at the forefront of our minds, there is no doubt a demand for qualified professionals that can handle these complex patient needs. While the sense of urgency for these services exists, especially as more and more healthcare consumers are resuming in-person appointments, unfortunately, there are processes in place that can create unnecessary roadblocks for practitioners.
Complying with the Council for Affordable Quality Healthcare’s (CAQH) behavioral health credentialing requirements are especially challenging. Unlike traditional medicine, treatments and therapies for conditions such as addiction are not as well understood by payers. This makes it more difficult to gain or maintain the credentials necessary to submit claims for therapy services.
Ninety percent of the time counselors and therapists apply for network status are denied! That’s a striking statistic, even for seasoned professionals, and everyone can agree that appealing denials and requesting payers review credentials in greater depth are a time consuming and expensive burden. On average, the time required for behavioral health credentialing of professionals is up to five times greater than for medical professionals because of nuances specific to the industry. The turnaround for completed enrollments is slower too, on average 180 days versus 120 days. In addition, some payers will only allow certain therapies for providers without advanced degrees. Because denials for behavioral health are common, therapists must understand which therapies a network will accept and focus on therapy-specific credentialing. In the current environment, practitioners should also ensure that Telehealth or virtual appointments will be covered for the safety of all.
So how can mental health providers stay ahead of enrollments and avoid credentialing-related denials? Outside assistance from experts like those at TriZetto Provider Solutions offers an end-to-end credentialing service that ensures continuous payer follow up and insight into enrollment status. Our credentialing professionals are devoted to helping providers gain and maintain their credentials. We understand the nuances associated with behavioral health credentialing and have direct relationships with all major payers. TPS allows you to do what you do best – manage patient care – by alleviating the burden of credentialing and making sure you never miss quarterly re-attestation deadlines.
If your mental health services are being denied, we are here to help. Learn how solutions from TriZetto Provider Solutions can help your practice simplify credentialing.
TriZetto Provider Solutions is a partner of EZClaim and can assist you with all your coding needs. For more details about EZClaim’s medical billing software, visit their website, e-mail their support team, or call them at 877.650.0904.
[ Contribution: The TriZetto Provider Solutions editorial team ]

Feb 9, 2021 | Administrative Safeguards, Cloud Security, Live Compliance, Medical Billing Software Blog, Partner
Ransomware hackers target medical billing companies, and it CAN AFFECT your entire company! (Ransomware is a type of malicious software designed to block access to a computer system until a sum of money is paid.)
Often out of one’s control, ransomware hackers target medical billing companies because of the tremendous value of the data. BUT, there are steps that CAN BE TAKEN to protect you, your company, and your patients and/or clients.
NetWalker Ransomware, for example, gained notoriety for targeting hospitals and healthcare providers with e-mails claiming to provide information about COVID-19. (The e-mail usually has an attachment that downloads the ransomware from a remote server when clicked on.) The thing is, this is very lucrative for identity thieves since medical records information sells anywhere from $1-$1000!
As the number of healthcare providers taking advantage of Telehealth continues to increase—now outnumbering in-person visits—the number of ransomware attacks continues to increase as well. This means Billers and Providers must be aware of the programs that are used on their machines and ensure necessary steps are taken to safeguard against hackers and attacks.
How can you protect yourself and/or your organization?
- Carefully monitoring where you store and enter your passwords can be extremely beneficial to help minimize the risk of a hack and keeping personal or patient information protected.
- Routine password changes and monitoring where you store and enter your passwords can be extremely beneficial to help reduce the risk of becoming a victim to a hacker. Passwords should be long, unique in characters, capitalization, and alphanumerical.
- Have you had an accurate and thorough Security Risk Assessment and/or penetration testing? If you haven’t completed an accurate and thorough security risk assessment, you could also be penalized under ‘willful neglect’ (this category alone is $50,000 per violation!) in addition to the higher risk of ransomware attacks.
- If you believe you might have revealed sensitive information about your organization, report it to the appropriate people within the organization, including network administrators. They can be alert for any suspicious or unusual activity.
- The strength of your passwords directly impacts your online security.
Live Compliance can help. They aggregate breaches which enables you to assess where personal data has been exposed. Dark Web scanning is built right into their Portal, and it allows you to keep an eye on employees whose information was involved in a breach, where the breach took place, and then suggest the next steps to take.
At Live Compliance, they make checking off your compliance requirements extremely simple and to ensure this doesn’t happen to you or your organization:
- Reliable and effective compliance
- Completely online, our role-based courses make training easy for remote or in-office employees
- Contact-free, accurate Security Risk Assessments are conducted remotely. All devices are thoroughly analyzed regardless of location. (Conducting an accurate and thorough Security Risk Assessment is not only required but is a useful tool to expose potential vulnerabilities, including those such as password protection.)
- Policies and procedures curated to fit your organization ensuring employees are updated on all workstation use and security safeguards in the office, or out of the office—all updated in real-time
- Electronic, prepared document sending and signing to employees and business associates
So, don’t risk your company’s future on ransomware hackers. Contact one of EZClaim’s partners, Live Compliance, especially since they are offering a FREE Organization Assessment to help determine your company’s status. E-mail them, visit their website at LiveCompliance.com, or call them at 980.999.1585.
For more information about EZClaim’s medical billing software, which provides a best-in-class product with correspondingly exceptional service and support, e-mail, visit their website, or contact them at 877.650.0904.
[ Article contributed by Jim Johnson of Live Compliance ]

Jan 11, 2021 | Electronic Billing, Partner, Waystar
With Medicare Advantage enrollment continuing to rise and more plans offering more benefits than ever, big changes are coming in 2021. This post will discuss the key changes to Medicare Advantage plans in the next year, program updates due to the COVID-19 public health emergency, and advice on how to navigate billing and reimbursement concerns.
For the first time in history, Medicare Advantage (MA) penetration has reached 40% of the total Medicare-eligible population. Currently, 25.4 million people are enrolled in Medicare Advantage (MA) plans, with a total Medicare-eligible population of 62.4 million, according to the Centers for Medicare and Medicaid Services (CMS). [ Link to report ]
With an aging population, enrollment in Medicare Advantage plans will only continue to grow (The Congressional Budget Office projects enrollment in these plans to rise to about 51% by 2030).
Medicare Advantage is an alternative to traditional Medicare that acts as an all-in-one health plan and is sold by private insurers. All Medicare Advantage plans must provide at least the same level of coverage as original Medicare, but they may impose different rules, restrictions, and costs. Most Advantage plans offer the same A and B coverage for the same monthly premium as regular Medicare plans, but also often include Part D prescription drug coverage, limited vision, and dental care, broader coverage, lower premiums, maximum out-of-pocket limits, and extra benefits—all of which expanded in 2020.
While this represents a distinct opportunity for many providers to be more profitable, growing enrollment also poses challenges. Medicare beneficiaries have more choice than ever before when it comes to selecting an MA plan.
According to the Kaiser Family Foundation (KFF), there are 3,148 Medicare Advantage plans available for individual enrollment for the 2020 plan year—an increase of 414 plans since 2019. The average beneficiary could choose among 28 plans in 2020. While the choice is great for the beneficiary, it adds complexity to healthcare providers’ revenue cycles, who need to navigate hurdles that vary by the plan in order to get reimbursed.
MA plans also tend to be more transient, meaning patients may switch often, even yearly if they choose through the open enrollment period. Providers must better manage every patient accordingly so they can maximize plan benefits. Doing so takes more effort, but the payoff can lead to profit.
CMS has clearly stated a goal to move from the current fee-for-service models toward value-based care. While the Medicare Advantage population grew by 60% from 2013 to 2019, the fee-for-service Medicare population only grew by 5%. The progress Medicare Advantage plans have achieved essentially creates an idea marketplace for beneficiaries. Enrollment costs are down and more plans than ever are offering new, innovative benefits. But what does this mean for providers?
So, how has COVID-19 affected Medicare Advantage plans? Well, the COVID-19 stimulus package, the Coronavirus Aid, Relief and Economic Security (CARES) Act, includes $100 billion in new funds for hospitals and other healthcare entities. The Centers for Medicare and Medicaid Services (CMS) made $30 billion of these funds available to healthcare providers based on their share of total Medicare fee-for-service (FFS) reimbursements in 2019, resulting in higher payments to hospitals in some states than others, according to KFF. Hospitals in states with higher shares of Medicare Advantage enrollees may have lower FFS reimbursement overall. As a result, some hospitals and other healthcare entities may be reimbursed less than they would if the allocation of funds considered payments received on behalf of Medicare Advantage enrollees.
In response to the COVID-19 emergency, many Medicare Advantage insurers waived cost-sharing requirements for COVID-19 treatment, meaning that Medicare Advantage beneficiaries will not have to pay cost-sharing if they require hospitalization due to COVID-19 (though they would if they are hospitalized for other reasons).
If a vaccine for COVID-19 becomes available to the public, Medicare is required to cover it under Part B with no cost-sharing for traditional Medicare or Medicare Advantage plan beneficiaries, based on a provision in the Coronavirus Aid Relief, and Economic Security (CARES) Act.
A Spotlight on Prior Authorization
Medicare Advantage plans can require enrollees to receive prior authorization before service will be covered, and nearly all Medicare Advantage enrollees (99%) are in plans that require prior authorization for some services in 2020, according to KFF. Prior authorization is most often required for relatively expensive services, such as inpatient hospital stays, skilled nursing facility stays, and Part B drugs, and is infrequently required for preventive services. Prior authorization can create barriers for providers and beneficiaries, but it’s meant to prevent patients from getting services that are not medically necessary, thus reducing costs for beneficiaries and insurers.
In a 2018 analysis, KFF found that four out of five MA enrollees—or 80%—are in plans that require prior authorization for at least one Medicare-covered service. More than 60% of MA plan enrollees require prior authorization before receiving home health services, and that percentage increases to more than 70% for skilled nursing facility and inpatient hospital stays.
The Families First Coronavirus Response Act (FFCRA) prohibits the use of prior authorization or other utilization management requirements for these services. A significant number of Medicare Advantage plans have waived prior authorization requirements for individuals needing treatment for COVID-19.
How Providers Can Prepare for a Medicare Advantage Boom
Medicare beneficiaries have more choice than ever before when it comes to selecting a MA plan. While the choice is great for the beneficiary, it adds complexity to healthcare providers’ revenue cycle. Healthcare providers will need to navigate new hurdles that vary by the MA plan in order to get reimbursed.
When beneficiaries change plans, it creates another challenge for providers. Historically, about 10% of MA enrollees change plans during open enrollment. Although this number seems low, even a small change in coverage can cause big problems for a healthcare provider’s revenue and cash flow. Billing the wrong insurance company leads to costly denials and appeals. Becker’s Hospital Review estimates that healthcare providers spend about $118 per claim on appeals. A study by the Medical Group Management Association found that the cost to rework a denied claim is approximately $25, and more than 50% of denied claims are never reworked.
Despite the challenges, providers don’t want to be left out of the MA boom. But how can they best prepare? Well, first off, healthcare providers need to ensure they are capturing accurate patient information. Next, they need to reevaluate workflows, so they are prepared to handle time-consuming prior authorizations. Additionally, healthcare organizations must consider how frequently they are re-running eligibility on patient rosters to make certain they do not miss a change in insurance coverage for patients under their care. Providers should re-run patient rosters monthly, so they have the most accurate benefit information. This will help them avoid unnecessary claim denials.
As MA continues to ramp up, the most successful providers will be those who work with a revenue cycle management partner that understands the nuances of Medicare reimbursement as well as the added complexities of MA.
With the acquisition of eSolutions, a leader in revenue cycle technology with Medicare-specific solutions, EZClaim’s ‘partner’, Waystar, so happens to be the first technology to unite commercial, government, and patient payments into a single platform, solving a major challenge and creating meaningful efficiencies. Billing Medicare, Medicare Advantage, and commercial claims from a single platform eliminates the hassle of managing multiple revenue cycle platforms and allows providers to get deeper AI-generated insights for faster reimbursement and increased value—for their organizations and their patients.
For more information about Waystar‘s platform, visit their website, or give them a call at 844.492.9782. To find out more about EZClaim‘s medical billing software, visit their website, e-mail their support team, or call them at 877.650-0904.
[ Article contributed by Waystar ]
Jan 11, 2021 | Electronic Billing, Health eFilings, Medical Billing Software Blog, Partner
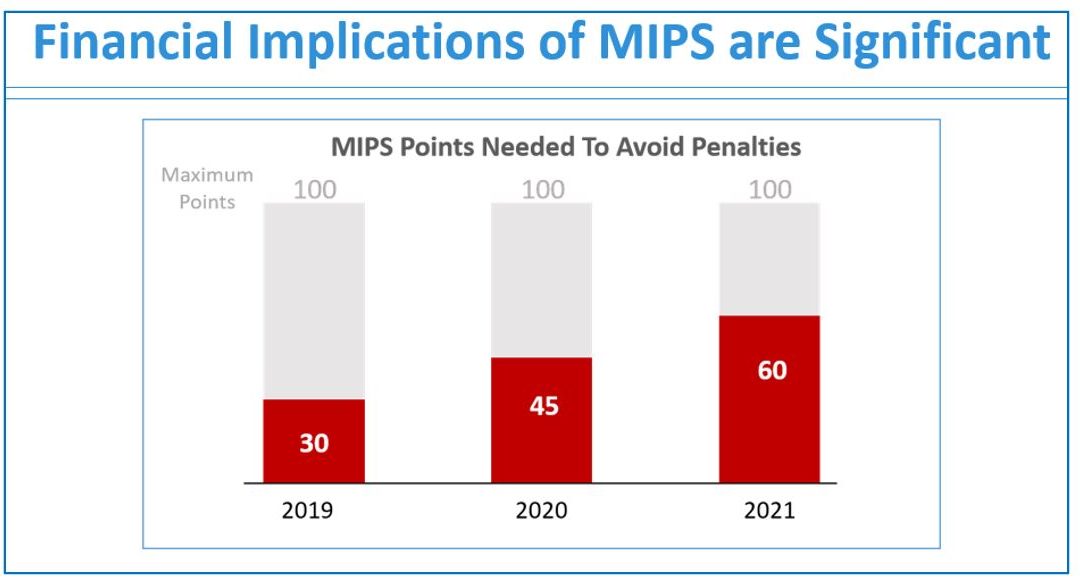
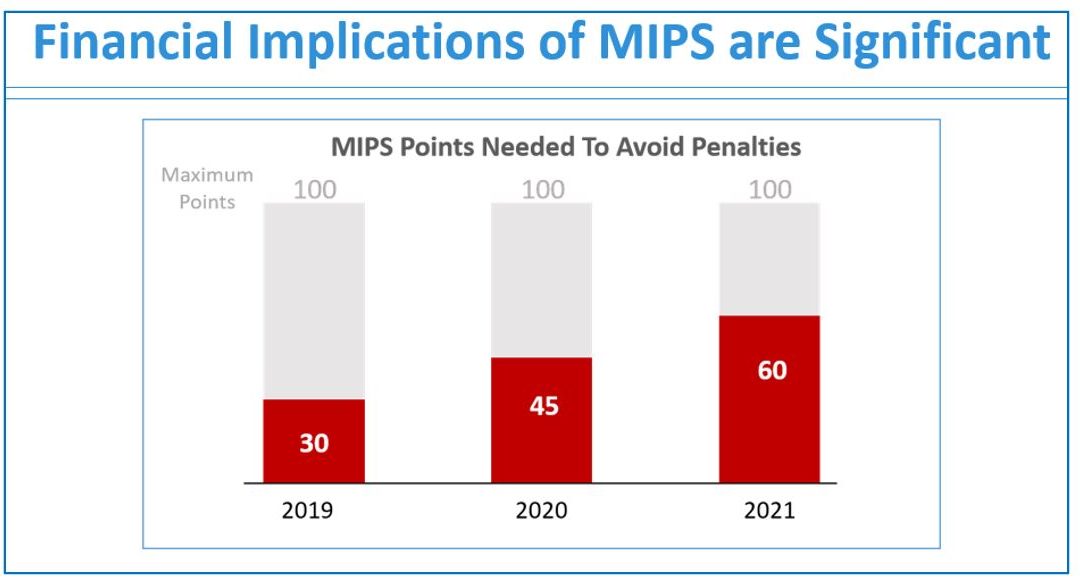
If you are not a MIPS expert (Merit-based Incentive System), your Medicare reimbursements may be decreased by 9% in the next year. However, it’s not too late to avoid the penalty for the 2020 reporting period, but you need to act now!
One of EZClaim’s partners, Health eFilings’ has ONC-certified software that completely automates the MIPS compliance process for you. The software will automatically extract the required data directly from EZClaim (and/or your EHR), and then proprietary algorithms will process the 9,000,000 possible combinations of quality measures for each clinician to identify which measures should be submitted to CMS (Centers for Medicare and Medicaid Services) to earn you the most points.
Need a MIPS expert? Well, Health eFilings is one of the best, and CMS has accepted 100% of their submissions on behalf of their clients. If you have completed your 2020 reporting, reach out to them, and learn how you can earn even more points in 2021.
For more information about EZClaim’s medical billing software, e-mail, visit their website, or contact them at 877.650.0904.
[ Article contributed by Sarah Reiter, SVP Strategic Partnerships, Health eFilings]