Jun 24, 2021 | Partner, RCM Insight
Have you ever been a bit overwhelmed when shopping around for all your medical practice needs? Of course! There are so many pieces required to meet all the HIPAA and reporting requirements, but it’s also about efficiency and ease of sharing information between clinicians to administrators. This can make the all-in-one Electronic Health Record (EHR) and Practice Management (PM) systems very tempting. Keep in mind, you will pay a hefty price for an all-in-one, which makes this a very simple decision for some practices. The good news: You have alternatives that still provide the same ease of sharing data through integration. I recently interviewed Dan Loch, President of EZClaim Software, LLC. EZClaim offers a stand-alone billing platform that offers several options for integration with clearinghouses and EHR’s. I asked Dan what he felt the biggest advantages were to using stand-along programs.
-
- Your practice will get the best of both worlds! Often practices will find a great EHR, but the billing side is not the best, or vice-versa. Using stand-alone programs that can talk to each other allows a practice to choose an EHR solution that is best for their clinicians AND a PM solution that is best for the billers and administrators.
- Typically, stand-alone systems are more ‘nimble’ in responding to industry and regulatory changes.
- Integrating multiple ‘best-in-class’ software packages creates an offering with much more in-depth capability.
If you are currently using separate EHR and PM solutions but the programs are not integrated – consider looking into this feature. This will relieve the burden of entering data twice. Start by verifying if the programs have an existing integration.
-
- If so, the hard part is done! Just ask what the process is to get set up and if there are any fees associated.
- If not, consider contacting your PM software vendor to inquire what formats they accept for EHR integrations. Once they provide the specs, work with your EHR to determine if you can export in the required format.
There is no single solution that works for every practice. If you’d like to learn more, check out this article from EZClaim ‘All-in-One’ or ‘Specialized’ Medical Billing Software? Which is Best? I hope that this information will help you weigh your options and find the right fit for your specific situation. If you have questions or would like some help determining what would be best, RCM Insight is here to help! Visit us at www.rcminsight.com and submit a request to chat on the Contact Us page.
Jan 11, 2021 | Electronic Billing, Health eFilings, Medical Billing Software Blog, Partner
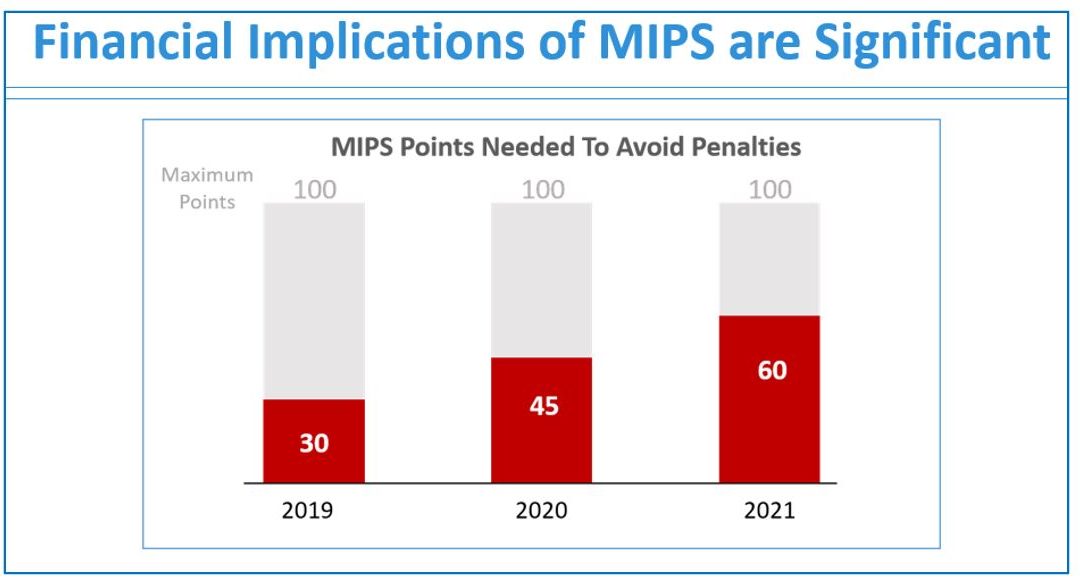
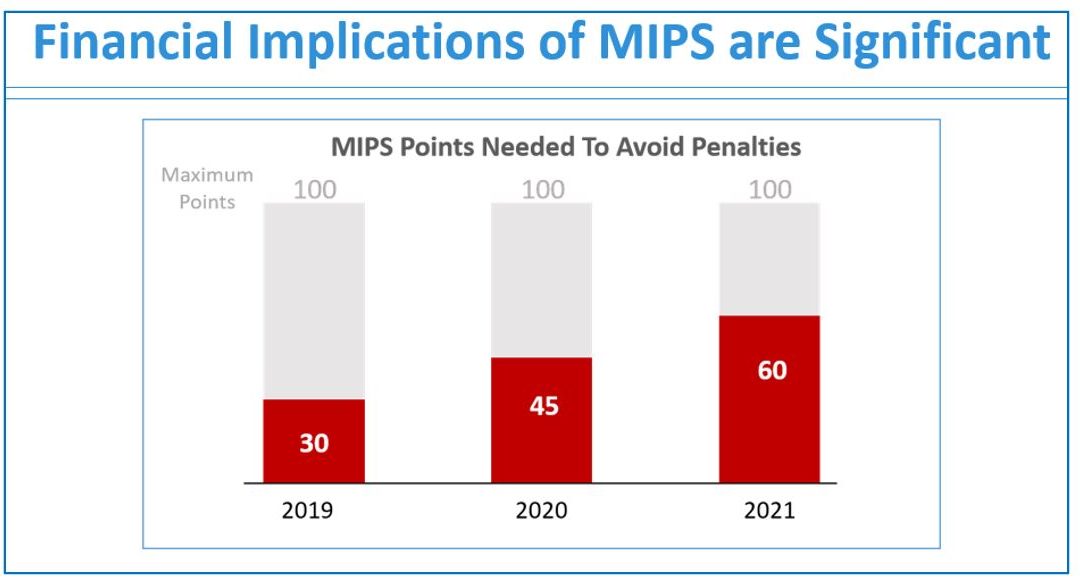
If you are not a MIPS expert (Merit-based Incentive System), your Medicare reimbursements may be decreased by 9% in the next year. However, it’s not too late to avoid the penalty for the 2020 reporting period, but you need to act now!
One of EZClaim’s partners, Health eFilings’ has ONC-certified software that completely automates the MIPS compliance process for you. The software will automatically extract the required data directly from EZClaim (and/or your EHR), and then proprietary algorithms will process the 9,000,000 possible combinations of quality measures for each clinician to identify which measures should be submitted to CMS (Centers for Medicare and Medicaid Services) to earn you the most points.
Need a MIPS expert? Well, Health eFilings is one of the best, and CMS has accepted 100% of their submissions on behalf of their clients. If you have completed your 2020 reporting, reach out to them, and learn how you can earn even more points in 2021.
For more information about EZClaim’s medical billing software, e-mail, visit their website, or contact them at 877.650.0904.
[ Article contributed by Sarah Reiter, SVP Strategic Partnerships, Health eFilings]

Nov 10, 2020 | Medical Billing Software Blog, Partner, Revenue, Support and Training, Waystar
 There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.
There are five ‘phases’ in the life cycle of a medical bill: Pre-appointment; Point of care; Claim submission; Insurance payment or denial; and Patient payment. This post will overview each of these phases, and could even be considered to be a “101-level” course on Revenue Cycle Management.
With high deductible health plans on the rise, the recent explosion of telehealth appointments due to COVID-19, and many other factors in play, it’s more important than ever for everyone to understand the life cycle of a medical bill, and how the process works. The healthcare revenue cycle is relevant not only to those who work in healthcare, but to the patient, too.
The revenue cycle is the series of processes around healthcare payments—from the time a patient makes an appointment to the time a provider is paid—and everything in between. One way to think of it is in terms of the life cycle of a medical bill. Although there are many ways this process can play out, this post will lay out a common example below:
1. Pre-appointment
For most general care, the first stage of the revenue cycle begins when a patient contacts a provider to set up their appointment. Generally this is when relevant patient information will begin to be collected for the eventual bill, referred to on the financial side of healthcare as a claim.
At this point a provider will determine whether the appointment and procedure will need prior authorization from an insurance company (referred to as the payer). Also, the electronic health record (EHR) used to help generate the claim is created, and will begin to accumulate further detail as the provider sends an eligibility inquiry to check into the patient’s insurance coverage.
2. Point of care
The next step in the process begins when the patient arrives for their appointment. This could include when a patient arrives for an initial consultation, an outpatient procedure, or for a follow-up exam. This could also include a Telehealth appointment.
At any of these events, the provider may charge an up-front cost. One example of this is a co-pay, which is the set amount patients pay after their deductible (if they are insured), however, there are other kinds of payments that fall into this category, too.
3. Claim submission
After the point of care, the provider completes and submits a claim with the appropriate codes to the payer. In order to accomplish that, billing staff must collect all necessary documentation and attach it to the claim. After submitting the claim to the payer, the provider’s team will monitor whether a claim has been been accepted, rejected, or denied.
[ Note: Medical coding refers to the clerical process of translating steps in the patient experience with reference numbers. The codes are normally based on medical documentation, such as a doctor’s notes or laboratory results. These explain to a payer how a patient was diagnosed and treated, and why. This information helps the payer decide how much of an encounter is covered under any given insurance plan, and therefore how much the payer will pay. ]
4. Insurance payment or denial
Once the payer receives the claim, they ensure it contains complete information and agrees with provider and patient records. If there is an error, the claim will be rejected outright and the provider will have to submit a corrected claim.
The payer then begins the review process, referred to as adjudication. Payers evaluate claims for accurate coding and documentation, medical necessity, appropriate authorization, and more. Through this process, the payer decides their financial obligation. Any factor could cause the payer to deny the claim.
If the claim is approved, the payer submits payment to the provider with information explaining details of their decision. If the claim is denied, the provider will need to determine if the original needs to be corrected, or if it makes more sense to appeal the payer’s decision.
Following adjudication, the payer will send an explanation of benefits (EOB) to the patient. This EOB will provide a breakdown of how the patient’s coverage matched up to the charges attached to their care. It is not a billing statement, but it does show what the provider charged the payer, what portion insurance covers, and how much the patient is responsible for.
5. Patient payment
The next phase occurs when the provider sends the patient a statement for their portion of financial responsibility. This stage occurs once the provider and payer have agreed on the details of the claim, what has been paid, and what is still owed.
The last step occurs when a patient pays the balance that they owe the provider for their care. Depending on the amount, the patient may be able pay it all at once, or they might need to work with the provider on a payment plan.
The above example represents one way the lie cycle of a medical bill can play out. Some of the ‘phases’ are often repeated. Because of the complexity of healthcare payments and the parties involved, there is not always a ‘straight line’ from patient care to complete payment. That’s why we call it the revenue cycle, and there are companies that provide systems for its management.
One of EZClaim’s partners, Waystar, aims to simplify and unify healthcare payments. Their technology automates many parts of the billing process laid out above, so it takes less time and energy for providers and their teams, and is more transparent for patients (Click here to learn more about how Waystar automates manual tasks and streamlines workflows.) When the revenue cycle is operating at its most efficient, providers can focus their resources on improving patient care—and that’s a better way forward for everyone!
For more information of how Waystar works together with EZClaim, click here.
[ Article and image provided by Waystar ]
———————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support, and can help improve medical billing revenues. To learn more, visit their website, e-mail them at sales@ezclaim.com, or call a representative today at 877.650.0904.
Oct 13, 2020 | HIPAA, Live Compliance, Medical Billing Software Blog, Partner
New HIPAA compliance requirements are coming!
In an effort to make the HIPAA Privacy Rule as easy to understand as possible, the Office for Civil Rights (OCR) has come up with a list of rules that clearly explain what Business Associates are now “directly liable” for. As OCR Director Roger Severino explains, “We want to make it as easy as possible for regulated entities to understand, and comply with, their obligations under the law.” The list consists of ten rules that, if failed to follow, can result in penalties and monetary fines.
[ Note: Check out our previous post to access this list ].
Immediate Requirements:
As we enter the fourth quarter of the year, you may be wondering what immediate requirements should a Business Associate complete before the end of the year?
One of the most important rules also includes information about Business Associates, and their need for proof of satisfactory assurance when the covered entity requests this of them. Satisfactory assurance is crucial, because it ensures the Business Associate is HIPAA compliant, and therefore, must also be in the form of a contract.
The Satisfactory Assurance contract is oftentimes outlined in the form of a questionnaire, and requires the Business Associate to disclose the date of completion for various compliance requirements.
These include distribution and completion of workforce HIPAA training, implementation and distribution of policies and procedures, Business Associate documentation, and completion of an annual HIPAA Security Risk Assessment.
Are You Prepared?:
If a Covered Entity requests this proof from your organization, would you be able to successfully complete it without outdated completion?
If you are uncertain that your organization would be able to easily and efficiently provide that documentation, you may be facing thousands of dollars in fines for each vulnerability!
HIPAA Compliance Myths:
False: The security risk analysis is optional for small providers: All providers who are “Covered Entities” under HIPAA are required to perform a risk analysis. In addition, all providers who want to receive MU, and MIPS incentive payments must conduct a risk analysis.
False: Our office uses the Cloud, so we don’t need a risk assessment: Even if you have a fully HIPAA compliant cloud vendor, your patient data (ePHI and PII) still must go through all your systems to get to the cloud. So, you are still required to perform technical, administrative, and physical security risk analyses.
False: Our EHR makes us compliant, so we’re fine: While your EHR may provide excellent privacy and security features, it definitely doesn’t exempt you from the HIPAA security requirements.
Live Compliance helps their clients meet the ever changing and complex HIPAA State and Federal regulations. They protect the information they are entrusted with, and ensure their clients pass any Health and Human Services audits. If you are unsure or need assistance, call Jim Johnson with Live Compliance at (980) 999-1585.
Live Compliance is a partner of EZClaim, a medical billing software company. For more details about their solutions, visit their website at ezclaim.com.

Aug 11, 2020 | Features, Medical Billing Customer Service, Partner
Which is the BEST kind of Medical Billing Software? “All-in-One” or “Specialized”?
When considering WHICH medical billing solution they should use, practices wonder which is best, an “all-in-one” solution or specialized software. Well, the following are a few important pros and cons to consider when making a choice between these solutions.
ALL-IN-ONE:
An “all-in-one” system tries to provide a single, comprehensive solution that offers functionality for the major areas of the practice—Practice Management (PM), Electronic Medical/Health Records (EMR/EHR), and Revenue Cycle Management (RCM)—accessed from one central point. It has features like clinical notes, patient information, and history, diagnosis and treatments, scheduling, appointment reminders, reports, patient educational resources, as well as a medical billing section.
PROS:
• Most of what a practice need is included in the system
• There is no need to be concerned with multiple integrations or vendors
CONS:
• Tends to have a higher ‘entry’ cost
• Usually designed for the “middle-of-the-road,” therefore sometimes doesn’t properly address specific needs of a practice
• Sometimes, the practice is left paying for additional customizations to fit their particular needs
SPECIALIZED SOFTWARE:
Specialized medical billing software, on the other hand, is particularly programmed to maintain billing details of tests, procedures, examinations, diagnoses, and treatments conducted on patients. However, many specialized software providers extend their scope to include features like practice management, scheduling, and other administrative and clinical functions (that are generally a part of EHR software systems) by partnering with other specialty software companies—creating a “best-in-class” solution.
PROS:
• Integrating multiple “best-in-class” software packages—each taking a much more focused approach—creates an offering with much more in-depth capabilities
• Usually are more ‘nimble’ in responding to industry and regulatory changes
• More ’scalable’ in supporting the growth of a practice
CONS:
• Most of the time the practice has to deal with multiple vendors
CONCLUSION:
Where “all-in-one” solutions offer a wide breadth of capabilities across the business, they usually also lack focus, depth, and sophistication. “All-in-one” solutions are usually only efficient in one area, with the other areas tend to be ‘compromised’ and not fully developed. Then, when it comes to flexibility, they tend to be slow to adapt to changing practice needs.
Specialized software, however, typically offer a more efficient experience, with each ‘component’ streamlined and designed with a specific purpose in mind. Their focus on limiting the software scope makes them flexible and easy to use.
EZClaim—a leading software package in medical billing and practice management—has made it easier for the medical practice to have the benefit of a “all-inclusive” solution. They have created the best of both worlds by taking on the responsibility of integrating the “best-of-breed” into a harmonized “best-of-class” offering that allows the practice to pick and choose for their specific needs. The seamless integration of partner products and services ensures the practice does not have to give up robustness and flexibility for a simplified “all-in-one” solution, and it further enhances the practice’s workflow.
As a specific example, one of EZClaim’s partners is TriZetto Provider Solutions (TPS), a provider that seamlessly blends claims processing with revenue management and analytics software, so the practice can get paid faster, and more accurately.
Today, the practice can get the benefit of all the power and ease of use of EZClaim’s medical billing software and all the access and security that is needed when dealing with personal records by using TPS—which includes patient access, claims and denials management, patient financials, and advisory services.
The powerful integration between EZClaim and TPS efficiently adds functionality to the practice. Now the practice can gain deeper insight into the claim lifecycle, and take the proper steps to improve the overall health of the practice. The right ‘integrated’ solution makes all the difference!
So, if your practice needs more confident billing, after payments, and more informed decisions, but the power of EZClaim and TPS to work for your practice with the integrated suite of revenue cycle solutions.
In addition to TPS, EZClaim has tightly integrated a variety of of ‘components’ to be able to offer an “all-inclusive” best-in-class solution for a medical practice’s needs: Electronic Health Records (EHR), Clearinghouse, statement and payment services, HIPPA compliance, claims scrubbing, appointment reminders, and inventory management. It has partnered with a variety of providers like QuickEMR, BestNotes, and PracticeFusion [ Click here for an entire list of EZClaim’s partners ].
It is important to note that an “all-in-one” solution does not usually include the Clearinghouse portion that TPS offers. The powerful integration between EZClaim, TPS, and EZClaim’s EMR partners, efficiently adds functionality to ANY practice!
If you are considering the best course of action to meet your practice’s needs, consider using EZClaim by downloading a FREE TRIAL or contact one of their product specialists today to explore all the options for how to best solve your practice’s operational challenges, and grow your business.
For details and features about EZClaim’s medical billing software, visit their website.