Apr 13, 2020 | Alpha II, Medical Billing Software Blog, Partner
One of our partners, Alpha II, is presenting a special webinar on COVID-19 billing changes on April 16, 2020, “COVID-19: Critical Coding and Regulatory Updates,” to provide the most up-to-date information on the coming changes to new procedures, diagnosis codes, telehealth updates, and changes to regulatory policies.
As guidelines for coding and billing of COVID-19 services are revised almost daily, rest assured Alpha II is working to implement these critical changes to regulations and coding guidance as quickly as possible by conducting near-daily promotions.
Here is a very brief summary of some of the updates we’ve implemented:
-
- Clarification of correct telehealth rendering POS and use of modifier -95
- Modification of diagnosis code edits for billing of COVID-19 symptoms from February 20 – March 31, 2020, and use of new diagnosis U07.1 for dates of service on or after April 1, 2020
- Addition of the new AMA CPT code 87635 effective March 13, 2020
- Addition of the new CMS CPT codes U0001 and U0002 retroactively effective February 4, 2020
- Modification for waiver of DME replacement requirements prior to March 1, 2020
- Modification for waiver of occurrence code 70 on SNF three-consecutive day stay validation prior to March 1, 2020
- Modification to LCD/NCD edits to relax rules related to respiratory-related devices and services
- Modification to Medicaid for the temporary suspension to prior authorization rules in PHE areas effective March 1, 2020
You can get all the latest COVID-19 specific updates here: https://www.alphaii.com/landing/covid19
Alpha II is an EZclaim partner that provides “Claim Scrubbing” for our medical billing software system. View our website for more details on this: https://ezclaim.com/partners/

Apr 13, 2020 | BillFlash, Partner
Medical billing managing collections during COVID-19 will be different than it was in the past. It has already changed a lot about how medical practices operate, and in a short amount of time. One thing that hasn’t changed, however, is that practices need to get paid in order to continue operating. This includes sending patients to collections when necessary.
Managing late or unpaid bills during economic uncertainty may require a different approach than you’re used to. Before you send patients to collections, make sure you take these steps first.
- Be upfront about payment expectations from the beginning
-
- You should already have a strategy in place regarding informing patients how much they owe for services. Stick to it. Many people are hoping for leeway on certain bills due to the economic impact of COVID-19, but gently remind your patients that for essential healthcare services to continue, practices need to keep revenue flowing, and that means billing will continue as usual.
- Set up payment plans
-
- If a patient is unable to pay a bill in full, help them set up a payment plan. BillFlash PlanPay lets you set up scheduled, automatic payments to be paid over a set period of time. This is the best option for both you and the patient because:
- The patient has a more manageable bill
- Your practice is more likely to be paid in full
- Setting up a payment plan shows your patients you’re willing to work with them. That’s usually all they need to be assured that you care.
- Send out multiple reminders
-
- Use whatever resources you have—email, phone, text, mail—to contact patients about balances they owe. Be courteous in your reminders, but firm. Most patients want to pay their medical bills. Often all they need is a simple reminder and an easy way to make the payment.
- BillFlash helps you manage all of this during the pre-collections phase to help ensure you are paid as quickly and completely as possible.
If none of these steps work, then it’s time to get collections involved.
What to Include in a Collections Letter
Include all the facts of the visit. This includes:
-
- Date of service
- Service provided
- Amount patient owes
- Payment options
Tone of the Letter
The right tone in your letter can do more to ensure payment and a continued relationship with the patient than anything else you include. You need to convey a sense of urgency, but without being overbearing and intimidating.
A few tips to keep in mind:
-
- Empathize with the patient. Simply saying “We understand you may be experiencing financial difficulties at this time” is more likely to get a response than a curt “final warning” threat.
- Explain why it is important for the patient to pay anyway. Example: Like any other business, our practice relies on revenue to thrive. In order to continue to provide these valuable healthcare services, patients need to pay their bills in full and on time.
- Offer a payment plan. Give patients one more opportunity to pay their bills in smaller chunks over a period of time to avoid having their accounts sent to collections.
We’re all experiencing difficulties during this global pandemic. The only way to get through it is to work together. Being upfront with patients about payment expectations and being willing to work with patients who have fallen on hard times will help all of us through this global health crisis.
BillFlash Collections Services can help you in managing collections during COVID-19, and simplify and streamline all your other collection processes for you, saving you the headache of exporting, importing, and working with a disconnected agency.
As an EZclaim ‘preferred’ partner, BillFlash is fully integrated with the EZclaim Premier billing application. For more details, view this informational video: https://www.rcm.billflash.com/ezclaim For more information about the EZclaim billing solution, view our website: https://ezclaim.com/
Apr 13, 2020 | Health eFilings, Partner
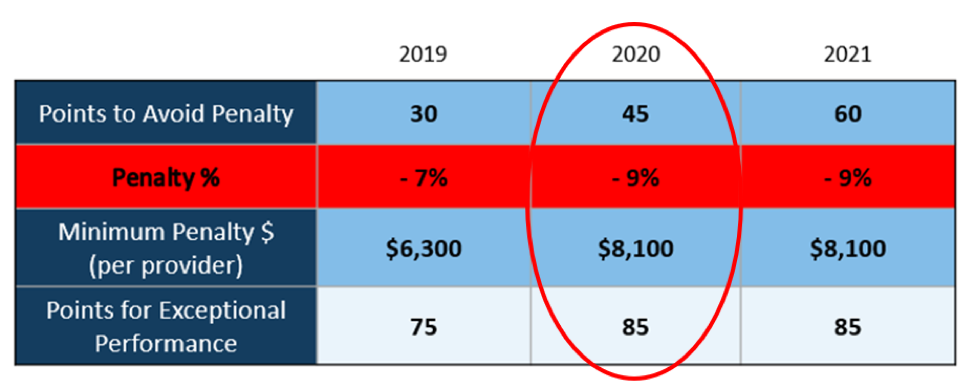
There WILL NOT be any changes to the MIPS Program in 2020, so all payers must be submitted and a minimum of 45 points must be earned to avoid the 9% penalty.
On March 23, 2020, CMS made it perfectly clear that MIPS Program is not going away in 2020. It also reiterated that the data requirements and thresholds in place for the 2020 program have not changed. Additionally, Promoting Interoperability and Improvement Activities must be done for the required durations, or no points will be earned for those categories.
To put this in context, while the stakes have been raised every year, the final ruling for the 2020 reporting period is the most complex to-date, further increasing the stress, burden, and financial risk for over 900,000 clinicians who bill Medicare Part B. Failure to comply or earn enough points for the 2020 reporting period will result in an automatic 9% penalty on every Medicare Part B claim paid for an entire year. This equates to a minimum of a $8,100 per provider hit to the bottom line.
Given the unprecedented time when everyone’s bottom line is at risk, now is the time to get a handle on what’s at risk with the MIPS program and proactively engage to ensure your bottom line is not further jeopardized by being assessed a 9% penalty. It can be challenging to know exactly what you need to do to earn points, optimize your score, and protect your Medicare reimbursements, as there are many commonly misunderstood aspects and nuances with the MIPS program.
So, with what is at stake and the inherent complexity in earning points, it is critical that you select the right methodology and partner who can help you maximize reimbursements and protect your bottom line. Not all reporting methodologies are the same.
Health eFilings‘ CEHRT is the best choice for a reporting partner. Their cloud-based ONC-certified software fully automates the process and does all the work without any IT resources, administrative support, and workflow changes from the practice. Health eFilings service is an end-to-end electronic solution that will save significant time, be a turn-key submission process, and maximize the financial upside for providers.
As more than 25% of the 2020 reporting period is behind us, now is the time to act while there is still plenty of time to positively impact your results and points earned.
Health eFiling provides the nation’s only fully automated solution for MIPS compliance and is integrated with EZclaim’s billing solution. Click on the following link for more details: https://healthefilings.com/ezclaim
[Contribution by Sarah Reiter with the Senior VP of Strategic Partnerships]
Mar 10, 2020 | Live Compliance, Medical Billing Customer Service
Whether you are a person new to medical billing or someone who’s been in the business for years, launching a new medical billing practice can be hard. Understanding the market, connecting with new clients, and knowing how to master your processes are challenges that you often learn as you go. Despite these challenges, it is rewarding to be out on your own growing a new company. Before you jump, let us help you understand some essential keys that you can research upfront and prepare yourself to get one step closer to being successful.
1. ONE BILLING PLATFORM VERSUS MULTIPLE PLATFORMS: First and foremost you must make a conscious decision to either focus on being an expert on an individual medical billing platform, like EZClaim or tackling multiple platforms. There are pros and cons of both: being an expert can make you extremely efficient in your use of the software’s billing and, scheduling features, however, it can also limit your client base to only one set of software users. Whereas having a basic understanding of multiple platforms can allow you a larger base of medical offices while limiting your ability to truly understand how best to serve each individual client’s needs.
Pro tip: Start and master one trusted billing program, and grow your options as your billing business grows.
2. GET CLEAR ON THE CLEARINGHOUSE: A new billing company owner does not want to be held to just one clearinghouse as options are key here. Having the ability to work with any or many would be an essential piece to your billing services, however, you still want to know the best clearinghouses in the business. Understanding which clearinghouses provide the best products and services and being able to recommend those services to your client upfront will make your life easier and their business run smoother. For this very reason, EZClaim has built its software around partnerships and integrations with the best clearinghouses to make working with the one you need easy.
3. COMPLY OR DIE (HIPAA Compliance): The third key to any start-up is first understanding the importance of HIPAA Compliance. Medical billing firms literally can come crashing down with any missteps, mistakes, or misunderstandings of this essential piece of the puzzle. It goes without saying that if you are going to choose a billing software be sure that they have partnerships built around making sure you are protected. You are also responsible to make sure the data is protected so your customer and their patient’s data is safe.
HIPAA Hint: Check out Live Compliance for further details on the topic.
There are many options available out there for your new medical billing practice, and we recommend doing your research. Within that research, you will find that EZClaim ranks very high in performance and comes in at a great price.
To learn about EZClaim go to our about page, sign up for a demo, and/or download a trial for free today!

Mar 10, 2020 | Live Compliance, Partner
An independent physician gastroenterology practice in Utah had to report a breach related to a dispute with a Business Associate to the Office for Civil Rights Department of HHS.
After the investigation into the breach, it was determined that the practice of Steven A. Porter, MD “had failed to complete an accurate and thorough risk analysis, and failed to implement security measures sufficient to reduce risks and vulnerabilities to a reasonable and appropriate level” and therefore, has agreed to pay a $100,000 fine.
In addition to the monetary penalty, the practice is required to implement a Corrective Action Plan (CAP). According to the investigation resolution agreement, the practice agreed to conduct a thorough Risk Analysis, the Practice must develop a complete inventory of all its categories of electronic equipment, data systems, and applications that contain or store ePHI, which will then be incorporated into its Risk Analysis and must complete a Risk Management plan. They must also revise and implement actionable policies and procedures, all of which should have been in place prior to the breach incident.
Have you ever read such headlines and doubted whether a small Billing Company or independent physician practice actually ever face penalties?
According to the Resolution Agreement, the practice must also completely reinvent its Business Associate process, and implement a strict protocol to ensure it’s Business Associates are HIPAA Compliant. In addition to ensuring their Business Associate relationships are accurate, the entire staff must undergo security and privacy training that stresses the use of Business Associate services and applications, disclosures to Business Associates that require a Business Associates agreement, or other reasonable assurances in place to ensure that the Business Associate will and can safeguard the PHI and/or the ePHI. This puts immense pressure on the Business Associates, such as Billing Companies, to ensure that they are HIPAA Compliant, but also independent physician practices to ensure their Business Associates, “down the chain” are also compliant. This is also known as gaining Satisfactory Assurance of vendor HIPAA compliance.
What can you do?
As we have stressed before, it is important for you to understand that every complaint or potential breach must be investigated by HHS/OCR. If you, a billing company, or another vendor, suspect a breach you must inform the covered entity (your client) and have a breach risk assessment completed to determine key factors and take action. Keep in mind, a business associate is a ‘person’ or ‘entity’. This means there is no Billing Company too small or too large to comply with the Federal HIPAA regulations. Again, if you haven’t completed an accurate and thorough security risk assessment prior to that, you could also be penalized under ‘willful neglect’. This category alone is $50,000 per violation!
What we do is keep this from ever being a worry for you! In fact, we have a 100% audit pass rate! For example, Live Compliance has easy to understand HIPAA breach notification training. We perform your security risk assessment and manage all your requirements, including business associates, in a clean, organized cloud-based portal. Don’t risk your company’s future, especially when we are offering a FREE Organization Assessment to help determine your company’s status. It’s easy, call us at (980) 999-1585, email me jim@LiveCompliance.com or visit LiveCompliance.com
[ Contributed by Jim Johnson, President of Live Compliance ].