Jun 20, 2022 | EZClaim
Good medical billing practices and procedures are critical to success, but without the proper solutions in place, they become challenging to get right. Far too often small, independent practices become caught up in a cycle of poor cash flow as—without the right partners or tools—their in-house medical coding and billing team become overworked and overwhelmed.
EZClaim works to bring powerful tools to, and make it easy for, small and mid-sized practices and RCM companies to submit clean claims every time easily and efficiently.
Claims that need to be resubmitted drain resources and delay payment as they have to be researched and corrected. There are two ways that unclean claims make their way back to billers:
Denied claims are claims that are processed but not paid by the payer. There are many reasons why a claim may be denied. These could include duplicate claims, uninsured services, missing information, insufficient authorization, late submissions, and other reasons. Your medical billing team must investigate the reason for denial to appeal it.
Rejected claims lack important information or are not in compliance with formatting or data requirements. The payer may not process these claims if the claim contains missing information or incorrect insurance policy numbers. These can be corrected and then resubmitted for processing.
Regardless of whether a claim was rejected or denied, you have a limited time to determine why the claim was not paid and resubmit it.
EZClaim gives you the tools and structure to submit clean claims the first time to avoid rejection in the first place. Your team can take steps at different points in the patient encounter to decrease the chance of a claim being rejected or denied.
Use custom templates and rules to identify common mistakes immediately
It is likely that there are specific billing and coding issues that your team finds continually—this is common in the industry. While many organizations are aware of common billing, code, and denial trends, they don’t have the tools to manage them. EZClaim allows you to create custom rules that review billing and code data, and flag errors for review. Automating as much of the claim review process as possible will ensure your time is used most efficiently.
Use a checklist before each appointment with the patient
Be sure to engage the patient before the appointment to stop potential claim issues from the very beginning—has their insurance or patient information changed recently? Using a scanner to collect patient information makes this process easier. Running an insurance verification is another important step.
Document coding and billing review criteria in a central knowledge base
RCM directors, coders and billers are experts in their industry, but this knowledge is not always documented. To ensure clean claims, there are many billing and coding guidelines that must be referenced. Training and reviewing claims can be difficult due to the constant changes in billing and coding requirements, information specific to your practice and payers, and staff turnover. Having a central place to document policies, procedures, and best practices will allow you to maintain accurate data and make sure that claims are filed correctly. Our partner, Live Compliance, offers solutions to make this easy.
Catch rejections and denials proactively with PM software
With claim status verification features, EZClaim can help you be proactive and catch new rejections as soon as possible. As payers continue to add rejection and denial reasons, EZClaim helps you find out where rejection and denial reason codes are coming from and determine the best way to respond to them.
EZClaim is a leading medical billing and scheduling software provider that combines a best-in-class product, with correspondingly exceptional service and support. For more information, schedule a consultation today, email our experts, or call at 877.650.0904.
May 14, 2022 | EZClaim
Reporting is a fundamental tool in EZClaim and key to medical billing success. With EZClaim’s powerful reporting capabilities, your business decisions can be informed by real-time data and not left to chance. From adjustment reports to patient demographics, EZClaim comes with a range of baseline reports that every biller needs to work cleanly and efficiently.
Why these reports are critical for your business
Accurate and timely reporting is crucial to maintain a full awareness of your business and address issues before they become critical. With the right reporting tool in place, you can avoid lost revenue, keep reimbursements high, and decrease denials.
EZClaim provides insight to key revenue cycle metrics and makes it easy to identify month to month trends. Whether it is a payments report that shows a sudden drop in collections or an aging report for claims that have not been paid in a month or longer, these reports allow you to identify problems and take action before it is too late.
The features that set EZClaim reporting apart
On demand reporting formatted your way
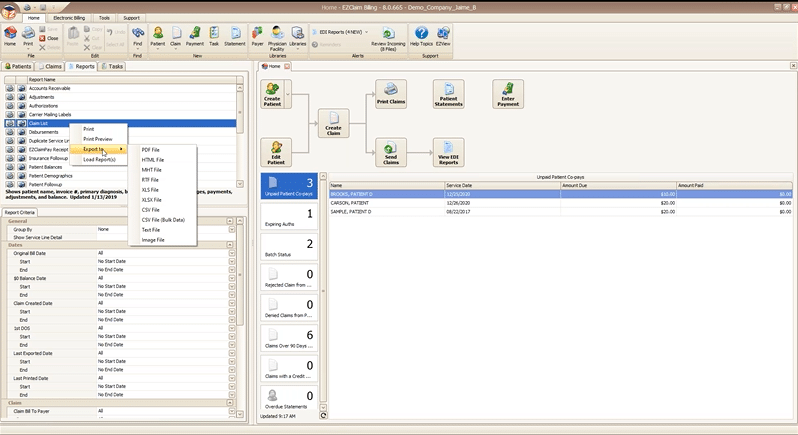
All EZClaim reports can be exported in a variety of formats so that you can open them directly in the format you most prefer. In two clicks you can preview and print a hard copy of any report, or export and open on your desktop.
Reports can be exported as a:
- PDF file
- HTML file
- MHT file
- RTF file
- CSV/XLS/XLXS (Excel) file
- Text file
- Image file
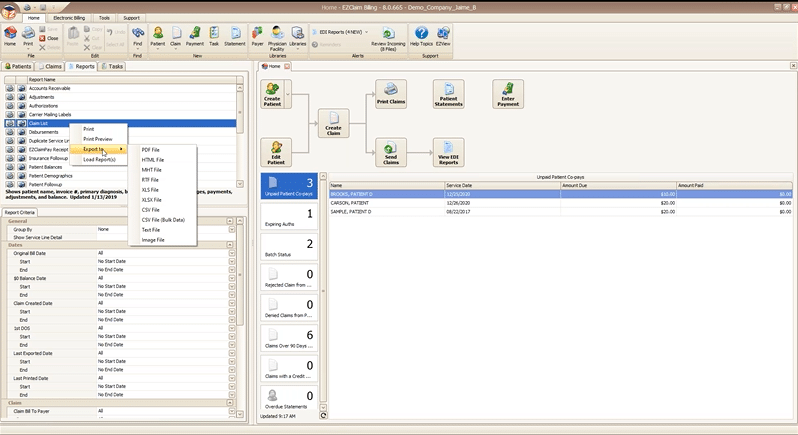
Getting just the data you want with report criteria
Every report in EZClaim can be tailored to show only the data you want by specifying report criteria. Report criteria parameters vary by report but aim to give you full control over what the report returns. For example, the “Claim List” report provides a list of claims and their associated details, such as invoice number, payments, adjustments, and more. This report provides a wide range of criteria options so that you can return only claims that, for example, fall in a particular bill date range, or claims for a specific payer. The best part is that you can combine as many criteria parameters as you need to zoom in on just data that you want.
With these features, EZClaim makes reporting powerful and flexible, by giving you the power to instantly create real time reports that are as focused or broad as needed, and then exported in the exact format that you need them.
If you are ready to learn more about EZClaim reporting or have any questions about our leading medical billing software, schedule a consultation today or get in touch with our experts.

Nov 11, 2021 | Health eFilings, Partner
MIPS Strategic Guide – How to Choose the Right Reporting Partner
Given the way the MIPS program has evolved, all healthcare practices regardless of size or specialty must evolve their approach to MIPS reporting to assure their success with the program. However, most clinicians do not understand or don’t have awareness of, the different reporting methods available to them and the impact the reporting method can have on their success with MIPS. With what is at stake financially, it is critical that you understand and select the right methodology and partner to maximize your MIPS points and protect your bottom line.
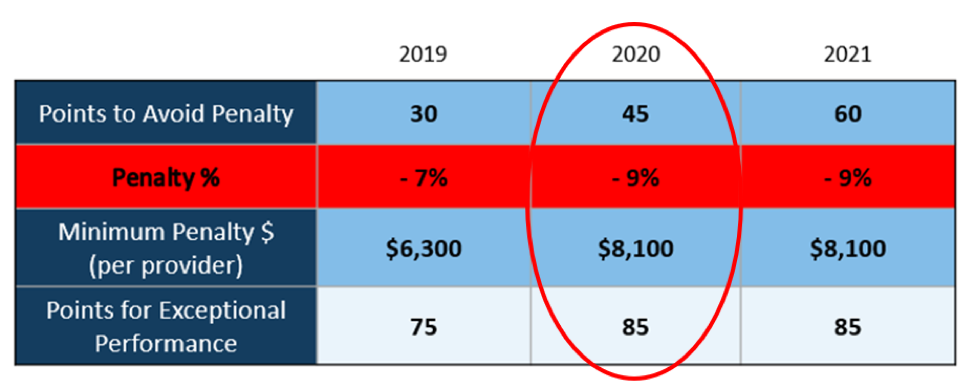
Many clinicians erroneously think that a registry is the only reporting option available to them or that they are required to use a registry. Or, they think that their EHR handles reporting for them. These misperceptions and general lack of awareness of the other reporting methodology will be detrimental to your ability to be successful with MIPS. And, given that 50% of all clinicians will be penalized annually by next year, the legacy reporting methods (registry or EHR) will not be able to fulfill enough of the reporting criteria to earn the minimum MIPS points needed to avoid the 9% reduction in Medicare reimbursements.
To help you determine if you are choosing the right reporting method and partner, we’ve identified the five most important factors to consider in order to increase your probability of avoiding the 9% penalty.
- Reporting Classification – is the reporting partner a CEHRT?
- Service Approach — Does the reporting partner use ONC certified software to do all the work with no IT resources, administrative support, or workflow changes?
- Quality Measures — Is the reporting partner certified by CMS to calculate all eCQMs, which earn significantly more points than registry measures?
- Benchmarking — Are proprietary algorithms used to assess the 9 million possible combinations of Quality measures to maximize earning MIPS points?
- Submission Method — Does the reporting partner submit a comprehensive electronic file directly to CMS to comply with reporting for all MIPS categories?
If you answer “no” to any of these questions, then the reporting partner you are working with will not be able to maximize the MIPS points you can earn. Given every MIPS point matters, because MIPS points determine your reimbursements and impact your bottom line, it’s time to consider a new strategy with a new reporting partner.
Health eFilings, a CEHRT, is the national leader in automated MIPS reporting. They utilize ONC-certified software to handle 100% of the tracking and reporting of the required data to CMS. And because their service is classified as an end-to-end electronic solution, you’ll also earn additional bonus points toward your MIPS score even though they are doing all the work. Health eFilings as your partner is the more effective and efficient reporting method so you will earn more points and, ultimately, receive higher reimbursements.
Learn more about how Health eFilings can help your practice here: https://healthefilings.com/ezclaim. Contact Sarah Reiter, sreiter@healthefilings.com, or 608.841.1866 to find out how to maximize your Medicare reimbursements and protect your bottom line.
About Health eFilings:
Health eFilings, a CEHRT, is the national leader in automated MIPS compliance and quality data analytics. Its services drive improved patient outcomes, optimized quality measures, and stronger financial results for healthcare practices. Their proprietary cloud-based ONC certified software is significantly more efficient and effective than any registry as it does all the work to extract, calculate, benchmark, format, and electronically submit MIPS data to CMS so clients avoid significant penalties and earn maximum reimbursements. And, you can have peace of mind knowing you are working with the best partner because CMS has accepted 100% of Health eFilings’ submissions. Learn more here: https://healthefilings.com/ezclaim
ABOUT EZCLAIM:
As a medical billing expert, EZClaim can help the medical practice improve its revenues since it is a medical billing and scheduling software company. EZClaim provides a best-in-class product, with correspondingly exceptional service and support. Combined, EZClaim helps improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.

Jun 24, 2021 | Partner, RCM Insight
Have you ever been a bit overwhelmed when shopping around for all your medical practice needs? Of course! There are so many pieces required to meet all the HIPAA and reporting requirements, but it’s also about efficiency and ease of sharing information between clinicians to administrators. This can make the all-in-one Electronic Health Record (EHR) and Practice Management (PM) systems very tempting. Keep in mind, you will pay a hefty price for an all-in-one, which makes this a very simple decision for some practices. The good news: You have alternatives that still provide the same ease of sharing data through integration. I recently interviewed Dan Loch, President of EZClaim Software, LLC. EZClaim offers a stand-alone billing platform that offers several options for integration with clearinghouses and EHR’s. I asked Dan what he felt the biggest advantages were to using stand-along programs.
-
- Your practice will get the best of both worlds! Often practices will find a great EHR, but the billing side is not the best, or vice-versa. Using stand-alone programs that can talk to each other allows a practice to choose an EHR solution that is best for their clinicians AND a PM solution that is best for the billers and administrators.
- Typically, stand-alone systems are more ‘nimble’ in responding to industry and regulatory changes.
- Integrating multiple ‘best-in-class’ software packages creates an offering with much more in-depth capability.
If you are currently using separate EHR and PM solutions but the programs are not integrated – consider looking into this feature. This will relieve the burden of entering data twice. Start by verifying if the programs have an existing integration.
-
- If so, the hard part is done! Just ask what the process is to get set up and if there are any fees associated.
- If not, consider contacting your PM software vendor to inquire what formats they accept for EHR integrations. Once they provide the specs, work with your EHR to determine if you can export in the required format.
There is no single solution that works for every practice. If you’d like to learn more, check out this article from EZClaim ‘All-in-One’ or ‘Specialized’ Medical Billing Software? Which is Best? I hope that this information will help you weigh your options and find the right fit for your specific situation. If you have questions or would like some help determining what would be best, RCM Insight is here to help! Visit us at www.rcminsight.com and submit a request to chat on the Contact Us page.
Apr 13, 2020 | Health eFilings, Partner
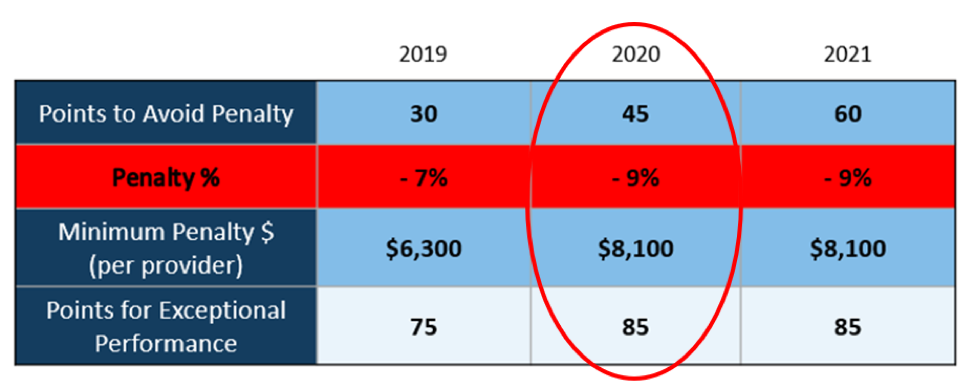
There WILL NOT be any changes to the MIPS Program in 2020, so all payers must be submitted and a minimum of 45 points must be earned to avoid the 9% penalty.
On March 23, 2020, CMS made it perfectly clear that MIPS Program is not going away in 2020. It also reiterated that the data requirements and thresholds in place for the 2020 program have not changed. Additionally, Promoting Interoperability and Improvement Activities must be done for the required durations, or no points will be earned for those categories.
To put this in context, while the stakes have been raised every year, the final ruling for the 2020 reporting period is the most complex to-date, further increasing the stress, burden, and financial risk for over 900,000 clinicians who bill Medicare Part B. Failure to comply or earn enough points for the 2020 reporting period will result in an automatic 9% penalty on every Medicare Part B claim paid for an entire year. This equates to a minimum of a $8,100 per provider hit to the bottom line.
Given the unprecedented time when everyone’s bottom line is at risk, now is the time to get a handle on what’s at risk with the MIPS program and proactively engage to ensure your bottom line is not further jeopardized by being assessed a 9% penalty. It can be challenging to know exactly what you need to do to earn points, optimize your score, and protect your Medicare reimbursements, as there are many commonly misunderstood aspects and nuances with the MIPS program.
So, with what is at stake and the inherent complexity in earning points, it is critical that you select the right methodology and partner who can help you maximize reimbursements and protect your bottom line. Not all reporting methodologies are the same.
Health eFilings‘ CEHRT is the best choice for a reporting partner. Their cloud-based ONC-certified software fully automates the process and does all the work without any IT resources, administrative support, and workflow changes from the practice. Health eFilings service is an end-to-end electronic solution that will save significant time, be a turn-key submission process, and maximize the financial upside for providers.
As more than 25% of the 2020 reporting period is behind us, now is the time to act while there is still plenty of time to positively impact your results and points earned.
Health eFiling provides the nation’s only fully automated solution for MIPS compliance and is integrated with EZclaim’s billing solution. Click on the following link for more details: https://healthefilings.com/ezclaim
[Contribution by Sarah Reiter with the Senior VP of Strategic Partnerships]