Jan 11, 2021 | Electronic Billing, Medical Billing Software Blog, Partner, Trizetto Partner Solutions
With a new year comes new medical coding changes.
After the examinations, x-rays, and surgeries, lives another major part of a physician’s day that happens behind the scenes. All the hard work needs to be processed through a successful claim submission, meaning that ultimately earning payment all boils down to one thing – coding. Evaluation and management codes, or E/M codes, are codes a physician uses to report a patient visit. This administrative task – a necessity for any physician – is often cumbersome and prone to errors. Most importantly, it uses up valuable time that could be better spent.
How many of us have experienced the “hurry up and wait” scenario? The type of appointment where you wait in a waiting room, then wait a little more in the exam room, then eventually get 10 minutes with your doctor…only to be rushed out so the next patient can be shuttled in. Unfortunately, it’s all too common. It’s safe to say that many patients could benefit from more face-to-face interaction with their providers.
Many people claim that payment for evaluation and management services is undervalued, specifically when it comes to ambulatory services. Additionally, it’s been argued that the fee schedule itself is not well-designed to support primary care, which requires ongoing care coordination for patients. Pressure existed to increase payment rates for ambulatory E/M services while reducing payment rates for other services. Thankfully, The Centers for Medicare and Medicaid Services (CMS) took notice. With the goal of increasing efficiencies to reduce unnecessary burdens, the “Patients over Paperwork” initiative was established. Per CMS, E/M codes make up 20% of total spending under the physician fee schedule. Part of this initiative aims to reduce the coding and documentation requirements for E/M codes, in turn giving physicians more time to spend with patients. In partnership with The American Medical Society (AMA), CMS worked to revise the rules for evaluation and management coding requirements. These changes were finalized in the 2020 Physician Fee Schedule (PFS) with an effective date of January 1, 2021.
So what exactly was revised? The E/M updates affect codes 99201 through 99215 and include the deletion of code 99201 along with revisions to the code selection for 99202 – 99215. Below is a summary of the revisions to E/M codes:
- Elimination of code 99201
- Decrease the burden of coding requirements
- Decreases the burden of documentation
- Decreases the need for audits
- Revises the definitions for Medical Decision Making (MDM)
- Revises the definition of time spent with the patient to total time including non-face-to-face for E/M services by a physician and other QHP
- Requires a history and/or examination when medically< necessary
- Offers a clear time ranges for each code for time spent with the patient
- Addition of a new 15-minute prolonged service code
- Clinicians will choose a code based on MDM or total time
These changes apply to office visits and other outpatient services. It’s noteworthy that these changes represent the first changes to the E/M codes in over 25 years! More importantly, the changes streamline the coding process, reduce clinician burden, and will allow physicians to put the focus back on patient care.
Billing and coding should always be top of mind, but it can be hard to keep up. This is why it’s critical for physicians, clinicians, coders, and billers to completely understand these changes. To help comprehension, the AMA released a checklist identifying ten steps to help the practices prepare for the upcoming changes that can be accessed here. To learn more about the medical coding changes and the summary of revisions, visit the AMA website.
TriZetto Provider Solutions is a partner of EZClaim, and can assist you with all your coding needs. For more details about the EZClaim medical billing solution, visit their website, e-mail their support team, or call them at 877.650.0904.
———————–
Note: This article is not a comprehensive overview and is NOT intended to provide coding advice, rather it is intended to highlight the new changes in effect and the need for physicians to ensure they have received the proper training for the upcoming changes.
[ Contributed by TriZetto Provider Solutions Editorial Team ]

Dec 14, 2020 | Live Compliance, Medical Billing Software Blog, Partner, Support and Training
There are a few HIPAA items to focus on RIGHT NOW—before the end of 2020!
The U.S. Department of Health and Human Services (HHS) has designated the “Health Insurance Portability and Accountability Act” (HIPAA) as the national standard for protecting the privacy and security of health information (in 1996). This led to the Health Information Technology for Economic and Clinical Health Act (HITECH), which has a provision in it for audits, and the HHS Office for Civil Rights is responsible for carrying out HIPAA audits, and responding to complaints and breaches. Ignoring them is not an option!
A Risk Assessment IS NOT Enough
A risk assessment is only one element of the compliance process. You must also “implement security updates as necessary and correct identified security deficiencies.” In other words, you must act via a Corrective Action Plan (CAP) and follow the required risk assessment process.
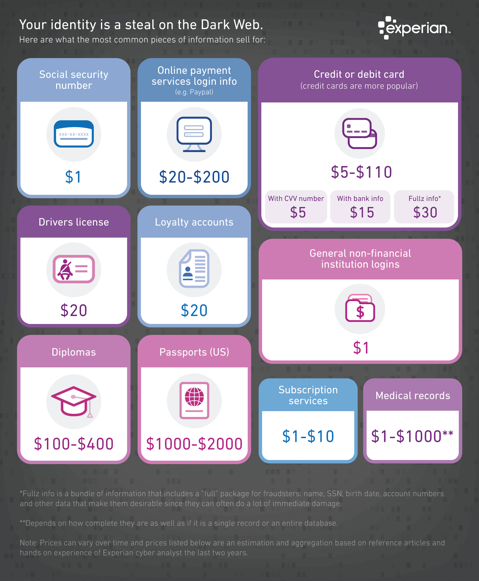
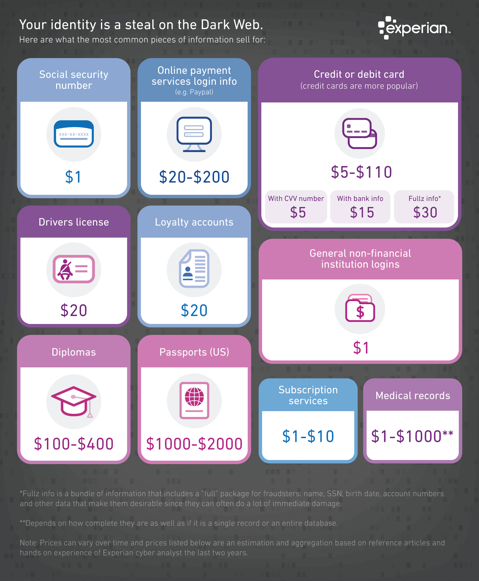
Dark Web
It is no secret that the “Dark Web” is a scary place to lose your information. So, what if it did happen and affected your entire company? Identity thieves get anywhere from $1-$1,000 for medical records, for each instance! So, how can you protect yourself and/or your organization?
Well, data breaches are becoming more common—sometimes which are out of your control—so carefully monitoring where you store and enter your passwords can be extremely beneficial to help minimize the risk of a hack and keeping personal or patient information protected.
One solution for this is the automatic Dark Web monitoring built into the portal of one of EZClaim’s partners, Live Compliance. Their solution helps keep an ‘eye’ on employees whose information was involved in a breach, and suggests next steps to take where the breach was found. Then, it allows your to conduct an accurate and thorough Security Risk Assessment. This is not only required, but is a useful tool to expose potential vulnerabilities, including those that involve password protection.
 So, what can I do to ensure this doesn’t happen to me or my organization? Well, Live Compliance makes checking off your compliance requirements extremely simple by providing:
So, what can I do to ensure this doesn’t happen to me or my organization? Well, Live Compliance makes checking off your compliance requirements extremely simple by providing:
● Reliable and effective compliance
● Completely online, our role-based courses make training easy for remote or in-office employees
● Contact-free, accurate Security Risk Assessments are conducted remotely. All devices are thoroughly analyzed regardless of location.
● Policies and procedures are curated to fit your organization, ensuring employees are updated on all workstation use and security safeguards in the office, or out. It is updated in real time.
● An electronic document is sent to employees and business associates
So, don’t risk your company’s future, especially when Live Compliance offers a FREE Organization Assessment to help determine your company’s status.
For additional details, call them at 980.999.1585, e-mail them, or visit their website at LiveCompliance.com
[ Article provided by Jim Johnson of Live Compliance ].
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call a representative today at 877.650.0904.

Dec 14, 2020 | BillFlash, Medical Billing Software Blog, Partner
If your New Year’s resolution is to get your practice back into tip-top shape, now is the time to determine your best ‘recipe’ for billing and payment success. In the spirit of the holidays, where award-winning recipes are part of the season, we have included our proven ‘recipe’ for billing and payment success:
INGREDIENTS:
– EZClaim billing software
– Patient statements
– Text & email eBills
– Online payments
– Payment plans
– Stored payments
– Automated payments
– Integrated Collection Services
PREPARATION:
Begin with EZClaim practice management software. Add integrated patient statements, and the ability to text and e-mail eBills. Then, mix in online payments, payment plans, automatic payments, and stored payments. Bake for 30-90 days, and watch your revenue rise! If needed, add a ‘dash’ of Integrated Collection Services to increase your serving amount.
Shape your billing and payment success by adding Pay Services, which will help your practice thrive financially in the new year (More details in this 60-second video). Also, view the Integrated Collection Services Video to learn how you can begin automating and simplifying the patient collections process.
OK, you might have found that a creative use of ‘recipe’, but you probably really want to see the Gingerbread cookie recipe in the photo. So, here it is:
Ingredients:
– 1/2 cups softened butter
– 1/4 cup packed brown sugar
– 1/4 cup granulated sugar
– 1 large egg
– 2 teaspoons ground cinnamon
– 1 tablespoon ground ginger
– 2-1/4 cups of flour
– 1/2 cup molasses
– 1 ‘dash’ of love
Preparation:
Cream butter and brown sugar together. Stir in molasses, then the egg. In a separate bowl, mix flour with all the spices. Stir in butter/sugar mix. If dough is too moist, add 2 tablespoons of flour.
Knead dough lightly, then chill for 40 minutes. Shape the dough into desired shapes. Bake at 350F until tops are ‘set’ (abut 8-12 minutes). Cool on a wire rack for at least 2 minutes before indulging! (If you don’t eat them all in one ‘sitting’, store them in an airtight container, at room temperature, for up to one month!).
[ Click here to download this delicious Gingerbread cookie recipe. (Also, we would love to see pics of your decorated cookies. Send them to sales@ezclaim.com) ].
As we approach the holiday season, EZClaim hopes that you are able to enjoy this time with your families!
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call a representative today at 877.650.0904.

Dec 14, 2020 | AMBA National Conference, Claims, Cloud Security, Denied Claims, EZClaim Cloud, EZClaim Premier, Medical Billing Customer Service, Medical Billing Software Blog
Deborah Rieser founded Spectrum Medical Billing Services in Anchorage, Alaska 15 years ago to make extra money to help with paying the family’s bills. Today, she owns a thriving medical billing service with a team of “twelve lovely ladies”—as she likes to refer to them—that services clients nationwide. Rieser originally selected EZClaim’s medical billing software platform—because of its pricing structure—to use for her medical billing service.
Over the years, since her original purchase, she has upgraded to each new EZClaim version, which adding new features and efficiencies. Recently, she has made the transition to EZClaim Cloud, and continues to use it exclusively today.
With team members nationwide, Rieser prides herself on training her billers on properly classifying billing for medical offices so that there are minimal insurance denials. She is very particular about this since one of the reasons Deborah began billing was the insurance qualification struggles she had for her daughter with Autism. So, accurate billing is ‘personal’.
Recently, we found time to interview Rieser about her start in the industry, the ups and downs of being a business owner, and what hard-fought expertise she has gained that might help others considering to start their own medical billing service.
EZCLAIM: When did you get into the medical billing industry and why?
RIESER: “I always had an entrepreneurial spirit, and I had an orchid business out of our house. Then my daughter, who was born with Autism, started working with an Occupational Therapist (OT), and they came to me to help with billing. I thought about it, and after a few weeks, I took it on. That was back in 2005.
“At that time, my daughter had over 75 volunteers and therapists in the community work with her from age three to age five, and had 50-60 hours a week of therapy. Today, she is a sophomore in university, has a boyfriend, is driving her car, and is thriving. From all of that, I have always felt the need to give back to the community for all their help. So, I used my business to take on other Pediatric, Occupational Therapy, Physical Therapy, and Speech Therapy clients, as well as, using my experience to help patients take care of their billing needs and get their bills paid by insurance.”
EZCLAIM: What are you passionate about when it comes to billing?
RIESER: “For me, the biggest thing that I am passionate about is seeing my clients [medical offices] getting paid from insurance claims. I also enjoy helping patients get properly classified during medical visits, so claims are accepted. I have learned a lot from the mistakes and errors that have led to denied claims. From my experience, I can help medical practices observe their approach to patients’ needs so that services qualify when billing insurance companies. Being able to offer that to my clients is very satisfying.”
EZCLAIM: What are some of the challenges you have had to overcome?
RIESER: “Originally, we grew word-of-mouth. I didn’t even want a website at first, but now I do have one. Going from one client to 65 is challenging because as your clients grow, your staff grows. Recently, I lost a client. You then have to decide what you’re going to do with your staff. The hardest part is that, for a business owner, your business consistently goes up and down. That fluctuation can be stressful. For me, I deal with that by going outdoors. My husband and I will go for a walk in nature and that will help relieve my stress.”
EZCLAIM: What advice would you offer others in the billing industry that have similar experiences?
RIESER: “If you’re starting your own business, make sure it’s one you love. Know that there will always be highs and lows. Also, be sure to price yourself accordingly. You can’t go too high or people will look elsewhere.
“I do want to step back and highlight that some of my billing practices only do 2-3 claims a week, and that’s why I love EZClaim. The price of the software. When I was growing, I was working on EZClaim “Advance,” which is being retired. So, when I started looking around at other software providers, they were billed on a ‘per provider cost.’ Fortunately, EZClaim “Cloud” billed based on the number of concurrent users, which worked for me.”
EZCLAIM: How has your relationship with AMBA (American Medical Billing Association) benefitted you?
RIESER: “I just joined last year in 2019, thanks to EZClaim and Dan Loch’s referral. I love that group. I joined their Facebook group because they have very useful information for us billers. I recommended that my team members join as well. They are good at supporting US-based companies and put the focus on supporting the group.”
EZCLAIM: What would you tell people who are wondering if EZClaim Cloud is right for them?
RIESER: “The transition to EZClaim Cloud was easy. I was worried about the providers and the tax ID’s, but it all was very smooth. I would add that customer support was very helpful. As daunting as moving things over felt, it was very smooth. I attribute that to the planning and support.”
EZCLAIM: What would you say would be a strength of someone who is good at billing and coding?
RIESER: “It is important to be a very good communicator, professional, out-going, and enjoy what you do. One must be able to communicate with providers over denials, success, celebrations, and always keep talking with the staff and the providers. Also, always try to put yourself in the patients’ shoes by offering patience and compassion. Lots of times patients don’t understand their benefits and why they are denied. So, try to explain in layman’s terms. They understand better and appreciate that. It ends up being a good connection with the patient, and benefits you as the biller, too.”
EZCLAIM: Final thoughts?
RIESER: “I am grateful to EZClaim for their services. As a business owner, you have to monitor expenses and things can add up fast. So, I am thankful for EZClaim Cloud and its pricing structure. That has helped Spectrum Medical Billing Services to grow and thrive.”
[ The above answers were paraphrased as closely as possible to the original answers given by Deborah Rieser on November 25, 2020 ].
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail them, or call a representative today at 877.650.0904.

Nov 10, 2020 | Alpha II, BillFlash, Claims, collections, Denied Claims, EZClaim Premier, HIPAA, Medical Billing Software Blog, Revenue, Support and Training
It IS POSSIBLE to improve medical billing revenues, and here are a few ways to do just that.
Healthcare practitioners, whether established or just starting out, have many overwhelming tasks: Managing a practice; Seeing patients; Working to staying up-to-date on administrative tasks; The whole host of compliance at the federal, state, and local level; and Overseeing the billing.
One of these that can lead to loss of revenue is not properly managing the medical billing, which can also lead to HIPAA fines and rejected claims. However, there is a solution: a medical billing system that balances the budget and optimizes revenues of medical practice.
EZClaim, an expert in the medical billing software market since 1997, provides a solution that improves the efficiency of an office’s billing process in many ways. The following are the primary reasons.
Reduce Coding Errors
Medical procedures become codes, codes become claims, and claims become revenue. Any error in this process can make claims to be denied, your workload can be increased, and revenue can be lost. To help in avoiding errors, it is essential to use billing software that offers the easiest implementation and access to descriptive diagnosis and treatment codes. EZClaim’s medical billing solution offers ease-of-use in coding, billing, and strong partnerships with Clearinghouses which act as an additional ‘safety net’ for catching errors.
Administrative Support
Most medical practices are a small team of people tackling a wide range of tasks, so when one cannot understand the function of the billing software, accessing reliable support is very important. EZClaim prides itself on having dedicated support experts available, and that was how the company was established. Founder and President Al Nagy has said, since day one, “We are a support company that happens to sell medical billing software.”
Maintain Industry Compliance
It is important to recognize that industry compliance and a practice’s revenue go hand-in-hand. Filing and batching inaccurate and non-HIPAA compliant claims can often be traced back to an outdated healthcare revenue management system. Conquering these tasks requires a focus on multiple fronts: A properly trained billing team, clear office procedures, patient payment policies, and a reliable medical billing company. These are all ways to help buttress against non-compliance and rejected claims.
Streamline Workflow
Recently, a study was done that showed almost 80% of medical bills contain errors. These incorrect medical claims often end up as lost revenue originally, not to mention the additional cost of resubmissions and collections. One of the best ways to resolve this problem for your practice is to make use of both well-trained, experienced billers and coders, combined with a competent medical billing solution that aids in catching these errors. EZClaim software features a library of standard validation, the ability to add custom validation, and integrates with Alpha II for full claim scrubbing.
Follow up
Errors will and do occur, so establishing a system for follow-up on all denials will close the loop and protect against lost revenue. Being consistent with the follow-up process, and having a medical billing solution that tracks these things will help close that gap.
Collections
Finally, probably the most important aspect that optimizes a practice’s revenue is to get paid. Portals and payment collection systems definitely help with this, but having collections integrated into the medical billing system is, of course, the best. EZClaim has pain-free payment processing integrated into their solution, called EZClaimPay. It solves all the problems associated with payment processing: Bank deposits, reconciliation, statements, changing fees, and ‘finger-pointing’ when there is a problem. EZClaimPay’s robust platform will greatly increase a practice’s collections success, and improve their revenue.
———————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support, and can help improve medical billing revenues. To learn more, visit their website, e-mail them at sales@ezclaim.com, or call a representative today at 877.650.0904.
[ Photo credit: Studioarz ]