Aug 26, 2021 | Partner, Waystar
Waystar’s newest guide investigates the state of denials and appeals in today’s healthcare landscape and explores how today’s most successful providers are redefining the core components of their denial and appeal process to grow revenue, streamline workflows and revitalize their approach to the process.
Denial and appeal management today
Like many administrative tasks further burdened by the impacts of the COVID-19 pandemic, denial and appeal management workflows dependent on manual processes are experiencing new strains on accuracy and productivity.
Last year a survey investigated how billing and administrative tasks were impacted by COVID-19, with 37% of surveyed providers reporting an increase in workloads due to issues with coding and requirements. An assessment of the general industry outlook found claim denial rates are at an all-time high, with 33% of surveyed hospital execs reporting concerns they are entering a “denials danger zone,” where rates grow to 10% or more.
Estimates put the cost of reworking denials as high as 20% of rev cycle expenses because on average they cost 4x as much to process than the initial claim. With so much strain already present on providers’ resources, many are turning to automation to ease the burden.
How automation elevates the process
Once a provider has been notified of a denied claim, steps are taken to identify whether or not it can be appealed. Many of the errors that cause denials come down to administrative issues that took place at the start of the claim lifecycle.
A recent analysis found 86% of the denials processed between July 2019 and June 2020 were avoidable. Analysis indicated that many of those issues stemmed from front-end errors related to benefit information, coverage detail, and shortcoming related to missing or invalid claim data.
While there’s a wide mix of problems that could cause a denial, with different providers experiencing a diversity of challenges depending on their location and patient population, they all face a common hurdle: the burden of manual denial management and appeal procedures put on administrative staff.
Like many other administrative processes, providers for the most part rely on a mix of manual and electronic procedures to handle denial and appeal management. But the industry’s continued reliance on manual procedures is beginning to have a negative effect.
How providers are transforming their approach to denial + appeal management
Studies have found that it costs about $118 in reworking fees to appeal a denied claim. These costs are exacerbated by the industry’s overall reliance on manual processes—a systemic issue many recognize yet fail to capitalize on. Indeed, while many providers see the promise automation can deliver on, they still face a number of considerations before pushing forward with implementing an automated solution.
And automation is a hot topic for providers for a very good reason—studies have demonstrated the US healthcare system could save as much as $16.3B by automating old or outdated processes. When it comes to denial and appeal management, the benefits are far-reaching, from improvements to productivity and a reduced strain on resources to huge boosts to claim accuracy and revenue recovery.
What to look for in a denial + appeal management solution
Leading-class solutions offer a wide selection of tools to provide a comprehensive approach to denial and appeal management, using customized, exception-based workflows to streamline the entire process and overturn a sizable increase in denials.
The appeal toolset a solution offers should make it easier to coordinate and use the info and data necessary to automatically process appeals and recover cash that would otherwise create productivity issues or unnecessary fees.
The solution’s ability to prioritize appeals based on cash value automatically lets staff concentrate on tasks that actually demand their attention, supporting them with additional tools like automatically generated payer-specific appeal forms and robust analytics capabilities that allow you to track and measure progress and problem areas.
Keeping disruptions at a minimum is key when considering your solution as well, so consider its ability to work efficiently with your existing systems and look for a partner that can demonstrate a strong history of seamless integrations.
Wrapping it up: why denial + appeal management solutions matters
A recent Waystar survey found 76% of providers categorized denials as their biggest RCM challenge. And the wider picture of healthcare reflects an industry struggling to solve a long-standing problem with manual processes and few answers.
Implementing an automated denial and appeal management solution is quickly becoming the optimal path forward for most providers, even if many have apprehensions about committing to the switch. But as new innovations cut down on the resources and time needed to implement the tech, the time is quickly approaching where the switch will be easier, and more vital, than ever before.
Click here to find out how Waystar can help fully automate the process and help you recover more revenue while reducing the burden on staff.
Heading to AMBA in October? Visit Waystar and EZClaim while you’re there! Stay tuned for more event details.
ABOUT EZCLAIM:
As a medical billing expert, EZClaim can help the medical practice improve its revenues since it is a medical billing and scheduling software company. EZClaim provides a best-in-class product, with correspondingly exceptional service and support. Combined, EZClaim helps improve medical billing revenues. To learn more, visit EZClaim’s website, email them, or call them today at 877.650.0904.
[ Contribution from the marketing team at Waystar ]

Feb 9, 2021 | Claim Status Inquiry, Claims, Denied Claims, Electronic Billing, Medical Billing Software Blog, Partner, Waystar
Reducing claim denials has long been a challenge for providers. In the worst case, denied claims end up as unexpected—and sometimes unaffordable—bills for patients. The challenge only seems to be growing. A recent survey conducted by the American Hospital Association (AHA) found that 89% of respondents had seen a noticeable increase in denials over the past three years, with 51% describing the increase as “significant.”
Minimizing loss will be top of mind for providers as the COVID-19 pandemic continues to put a strain on their resources, and minimizing or preventing denials will need to be a core part of that strategy. With that in mind, we’re offering four tips to help guide revenue cycle strategies for better denial reduction in 2021.
1. Analyze and Assess
In order to achieve and maintain a healthier denial rate, it’s vital to have a good handle on the factors creating problems in the first place. Keep the following in mind as you start to structure your analysis:
- Review key performance indicators: Take a look at which metrics are being used to benchmark success or failure and see if it’s time for a refresh
- Evaluate workflows: It’s important to have a clear understanding of how your team operates, and that you can detail workflows as step-by-step processes
- Assess tools: Inventory the software you’re using and discuss with your team how it helps or hinders them
- Staff efficiency: Consider the number of team members and resources involved in each step of the denial management process
It’s also important to talk to staff. Your team can offer invaluable insight on what is and isn’t working to help you develop a more comprehensive understanding of the shape and scope of the systemic issues contributing to your denial rate.
2. Reduce Errors Upfront
Eligibility, registration, and authorization errors remain the greatest cause of denials and write-offs, so a good first step is to focus on being proactive instead of reactive. Often, it’s easy to get into a routine where errors are only addressed after they occur. But incorporating tech to verify coverage and benefit accuracy in advance can lead to higher efficiency and much less manual labor spent to correct those issues later on.
Similarly, a recent AHA report found a failure to obtain prior authorization to be one of the most common reasons for a claim to be denied by a commercial health plan. In another recent survey, the American Medical Association found that 86% of providers surveyed were struggling with a high administrative burden created by prior authorizations.
Recent innovations have made the process simpler than ever. The right prior authorization solution can automate the process and make it simpler, smarter, and much less labor-intensive, reducing manual input errors and preventing denials.
3. Cut Down on Manual Labor
Claim denials are often the result of staff trying to keep track of a seemingly overwhelming number of rules and regulations while juggling various systems and filing requirements. When your staff is overburdened, it’s that much easier for them to make simple errors or miss deadlines.
There are numerous tools available for teams who are either struggling with paper-based processes or databases without automation. With an AI-powered solution, you can streamline a number of time-consuming tasks while simultaneously automatically ensuring you’re identifying missing data or claim errors that can be corrected before they’re submitted.
It’s also a good idea to review any potential new tools with your team. Their insight will help you properly determine which solutions will actually improve their workflows, and which could prove an expensive time sink.
4. Use Stronger Reporting Tools
Accurate and in-depth reporting should be core to your strategy. Effective reporting tools let you quantify and assess the issues that influence your denial rate, allowing you to easily spot persistent workflow errors or other systemic problems that can create extra work or strain resources.
New tools powered by AI and machine learning offer more robust reporting options than ever, with advanced analytics and visualization capabilities that make it easy to explore complex data sets or identify trends. Mountains of information can now be easily managed and measured, giving you access to operational insights that will help you better understand problem areas and identify opportunities for improvement.
The Wrap-up
With the right tools, a solid strategy, and expert guidance, you can take a proactive approach to reducing claim denials. Our automated tools make it easy for your team to streamline their workflows while reducing errors and administrative costs. With Hubble, our AI and RPA platform, you can unlock the insights you need to reduce your denial rate and increase cash flow.
Waystar, a partner of EZClaim, also offers a number of front-end solutions to help you take a more proactive approach to your denial rate. Click here to learn more about how Waystar can help you with reducing claim denials and claim management. For more information about Waystar’s platform, visit their website, or give them a call at 844.492.9782.
To find out more about EZClaim’s medical billing software, visit their website, e-mail their support team, or call them at 877.650-0904.
[ Contribution: Waystar ]
Oct 12, 2020 | Medical Billing Software Blog, Partner, Revenue, Waystar
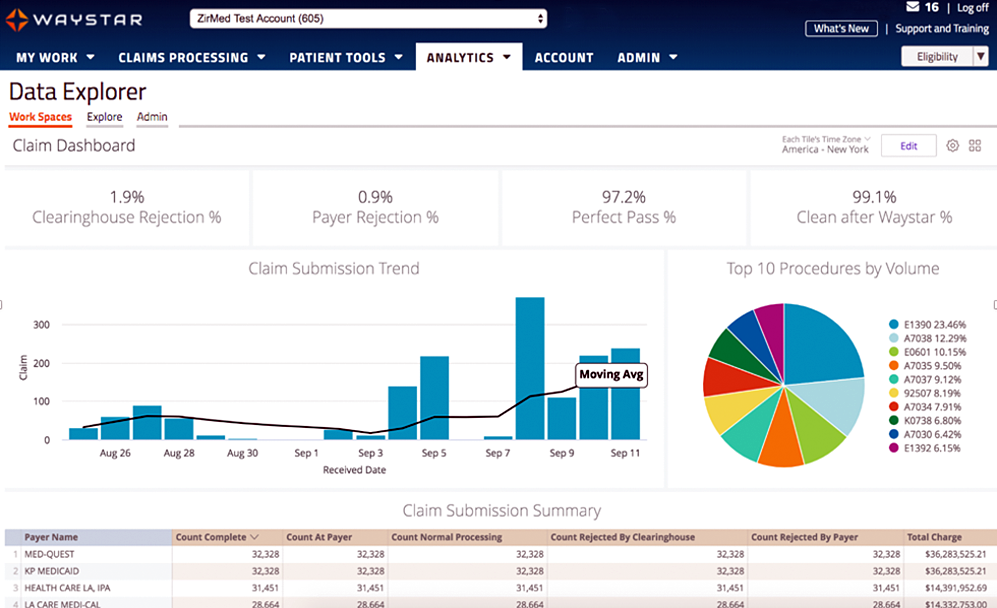
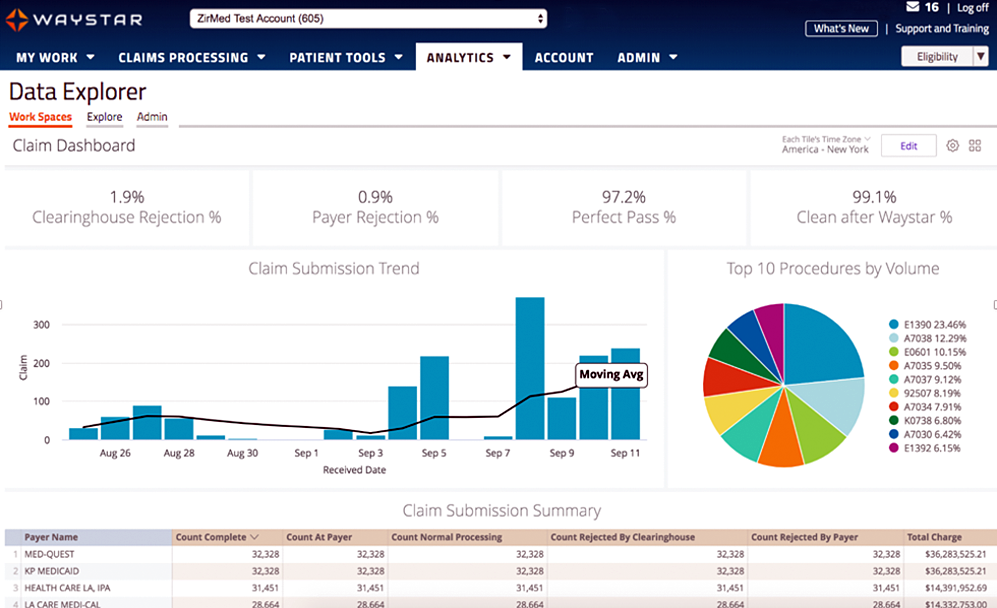
Today’s healthcare landscape faces truly unprecedented challenges, which means it’s more important to get the most out of your analytics to develop more informed, strategic decisions. There’s a deep well of data that each revenue cycle feeds into, which if properly analyzed, can help organizations operate at their most efficient and effective. Here are the four stages of data analytics workflows that are key to developing those actionable insights: A “Trigger,” or the point in your revenue cycle that sets up the call for deeper analysis; “Interpretation” of data to determine root causes and identify appropriate next steps; “Intervention” to improve specific metrics; and “Tracking” of said metrics to chart success in achieving desired outcomes.
So, let’s examine what a successful version of each stage looks like:
Trigger:
The trigger occurs when you notice something that needs further investigation. With the right analytics tool you can easily access all of your key performance indicators, financial goals and more, providing the visibility you need into your rev cycle. When something looks amiss or needs improving, you can drill down to the level that shows what’s really going on.
Interpretation:
Even a wealth of data amounts to nothing without an efficient way to process and communicate key takeaways. You’ll need to equip your team with access to concise reports, smart visualizations and relevant historical data in order to get them to the insights that drive action.
Intervention:
Now is the time to take action. Intervention is ultimately tied directly to your ability to drill down into the data underlying problematic areas of your revenue cycle and clearly communicate takeaways with your team. Success at this stage depends on designing a plan based on your best understanding of underlying issues and the most effective way to address them.
Tracking:
Your intervention plan is built on KPIs that naturally intertwine with the way you measure success across your revenue cycle. With proper implementation and tracking, running with the analytics cycle can become a simple addition to your everyday workflow. More than delivering on your initial goals, the true power of analytics is the ability to deliver repeat value on your initial investment.
Wrap Up
A strong analytics solution does more than deliver a more fully developed picture of your revenue cycle performance. It provides actionable business intelligence, cuts down on time between analysis and action, and lessens the strain on your IT department.
Waystar is a ‘partner’ of EZClaim, and provides analytics for a practice using their medical billing software. For more details about EZClaim’s products and services, visit their website: https://ezclaim.com/
To learn more about how Waystar can help you harness the power of your data, call their main office at 844-4WAYSTAR, or call sales at 844-6WAYSTAR.
[ Contributed by Waystar ]
Sep 10, 2020 | Electronic Billing, Medical Billing Software Blog, Partner
In the wake of the COVID-19 pandemic, Telehealth adoption has exploded, and there are six revenue cycle metrics to track.
Many patients are prohibited or reluctant to venture out for on-site care. The combination of relaxed regulations and expanded payment parity for appointments has made virtual meetings easier and more attractive for providers, who are turning to these technologies to stay engaged with patients—and maintain cashflow. Dr. Robert McLean, a former president of the American College of Physicians, recently said, “this crisis has forced us to change how we deliver health care more in 20 days than we had in 20 years.”
A new industry report predicts that the number of Telehealth visits in the US will surpass one billion by the end of the year, and speculates that nearly half of those visits will be related to COVID-19. At Waystar, we have been closely monitoring claim trends and are seeing this growth firsthand. In fact, the volume of Telehealth claims on the Waystar platform has grown by more than 100 times since mid-March. On two particular days in late April, they accounted for more than 15% of our total daily claim volume. Before COVID-19, they would have accounted for less than one percent!
For many providers, this shift will require new revenue cycle strategies to meet growing patient demand without overwhelming clinicians and administrative teams—or already strained operating budgets. It’s important to remember this is still very much an evolving care delivery model with the opportunity for errors on the part of both payers, providers, and administrative staff. For this reason, revenue cycle professionals should diligently monitor claims to ensure proper adjudication, identify learning opportunities, and uncover areas for operational improvement.
Below, we’ve listed six core Telehealth-related metrics you should regularly track to ensure billing accuracy, maximize payer reimbursement, and reduce claim rejections and denials. For more on how to best navigate the evolving telemedicine landscape, check out our resource hub here.
To report on Telehealth-related claims, you’ll first need to identify and isolate claims containing Telehealth procedure codes. See CMS’ Telehealth code list to identify the specific procedure codes and modifiers that apply to your organization.
Payer Analysis:
1. Payer Telehealth claim rejections by volume and/or billed amount
2. Payer Telehealth claim denials by volume and/or billed amount
If your Telehealth claims are being denied or rejected, do you know which specific payers are doing so at the highest rate? Drill down to discover the specific reason codes payers are attaching to rejections and denials so you can better understand payer-specific rules and avoid these oversights in the future. In some cases, you may identify trends that warrant a call to the payer to correct.
Provider Analysis:
3. Telehealth claim volume by the provider
Review this claim volume by individual provider. If you notice providers within your organization generating a much lower volume of Telehealth claims than peers, perhaps they could benefit from additional training on Telehealth technology and use cases.
Ensuring Billing Accuracy:
4. Telehealth claim rejections by biller/team
5. Telehealth claim denials by biller/team
Are certain billing personnel or teams producing higher denial or rejection rates than others? Keep a close eye on these trends and remember most of this is new for everyone. If some team members are seeing more rejections or denials than they should, it could be a great opportunity to hold training and collaborate on strategies for success.
Maximizing Reimbursement:
6. Telehealth claim volume by procedure code
Which Telehealth codes are you using? Each code reimburses at a different rate, so choosing the wrong ones could leave money on the table. Be sure to read up on CMS’ requirements (check out their fact sheet and code list) to ensure you’re choosing the appropriate code(s) on each Telehealth claim.
Waystar Analytics
You have all the data you need to drive informed decision making and improve financial performance—you just need the right analytics tool in your corner. Our new Waystar Analytics solution offers a pre-built Telehealth dashboard that can help you easily interpret, share all the metrics above, and track these revenue cycle metrics. Click here to learn more about Waystar Analytics and how it can deliver the insights you need during this time of transition.
[ By Waystar ]