Jun 20, 2022 | EZClaim
Good medical billing practices and procedures are critical to success, but without the proper solutions in place, they become challenging to get right. Far too often small, independent practices become caught up in a cycle of poor cash flow as—without the right partners or tools—their in-house medical coding and billing team become overworked and overwhelmed.
EZClaim works to bring powerful tools to, and make it easy for, small and mid-sized practices and RCM companies to submit clean claims every time easily and efficiently.
Claims that need to be resubmitted drain resources and delay payment as they have to be researched and corrected. There are two ways that unclean claims make their way back to billers:
Denied claims are claims that are processed but not paid by the payer. There are many reasons why a claim may be denied. These could include duplicate claims, uninsured services, missing information, insufficient authorization, late submissions, and other reasons. Your medical billing team must investigate the reason for denial to appeal it.
Rejected claims lack important information or are not in compliance with formatting or data requirements. The payer may not process these claims if the claim contains missing information or incorrect insurance policy numbers. These can be corrected and then resubmitted for processing.
Regardless of whether a claim was rejected or denied, you have a limited time to determine why the claim was not paid and resubmit it.
EZClaim gives you the tools and structure to submit clean claims the first time to avoid rejection in the first place. Your team can take steps at different points in the patient encounter to decrease the chance of a claim being rejected or denied.
Use custom templates and rules to identify common mistakes immediately
It is likely that there are specific billing and coding issues that your team finds continually—this is common in the industry. While many organizations are aware of common billing, code, and denial trends, they don’t have the tools to manage them. EZClaim allows you to create custom rules that review billing and code data, and flag errors for review. Automating as much of the claim review process as possible will ensure your time is used most efficiently.
Use a checklist before each appointment with the patient
Be sure to engage the patient before the appointment to stop potential claim issues from the very beginning—has their insurance or patient information changed recently? Using a scanner to collect patient information makes this process easier. Running an insurance verification is another important step.
Document coding and billing review criteria in a central knowledge base
RCM directors, coders and billers are experts in their industry, but this knowledge is not always documented. To ensure clean claims, there are many billing and coding guidelines that must be referenced. Training and reviewing claims can be difficult due to the constant changes in billing and coding requirements, information specific to your practice and payers, and staff turnover. Having a central place to document policies, procedures, and best practices will allow you to maintain accurate data and make sure that claims are filed correctly. Our partner, Live Compliance, offers solutions to make this easy.
Catch rejections and denials proactively with PM software
With claim status verification features, EZClaim can help you be proactive and catch new rejections as soon as possible. As payers continue to add rejection and denial reasons, EZClaim helps you find out where rejection and denial reason codes are coming from and determine the best way to respond to them.
EZClaim is a leading medical billing and scheduling software provider that combines a best-in-class product, with correspondingly exceptional service and support. For more information, schedule a consultation today, email our experts, or call at 877.650.0904.
May 14, 2022 | EZClaim
Reporting is a fundamental tool in EZClaim and key to medical billing success. With EZClaim’s powerful reporting capabilities, your business decisions can be informed by real-time data and not left to chance. From adjustment reports to patient demographics, EZClaim comes with a range of baseline reports that every biller needs to work cleanly and efficiently.
Why these reports are critical for your business
Accurate and timely reporting is crucial to maintain a full awareness of your business and address issues before they become critical. With the right reporting tool in place, you can avoid lost revenue, keep reimbursements high, and decrease denials.
EZClaim provides insight to key revenue cycle metrics and makes it easy to identify month to month trends. Whether it is a payments report that shows a sudden drop in collections or an aging report for claims that have not been paid in a month or longer, these reports allow you to identify problems and take action before it is too late.
The features that set EZClaim reporting apart
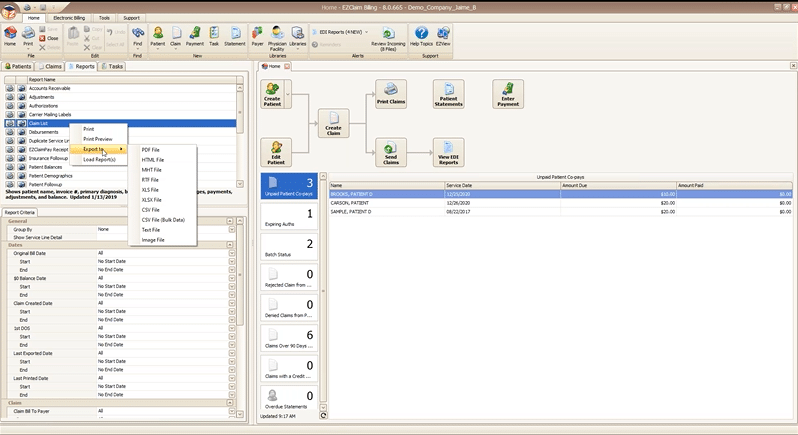
On demand reporting formatted your way
All EZClaim reports can be exported in a variety of formats so that you can open them directly in the format you most prefer. In two clicks you can preview and print a hard copy of any report, or export and open on your desktop.
Reports can be exported as a:
- PDF file
- HTML file
- MHT file
- RTF file
- CSV/XLS/XLXS (Excel) file
- Text file
- Image file
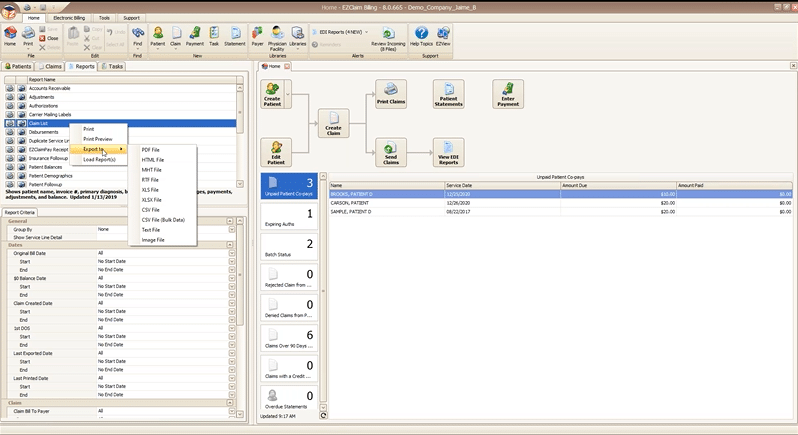
Getting just the data you want with report criteria
Every report in EZClaim can be tailored to show only the data you want by specifying report criteria. Report criteria parameters vary by report but aim to give you full control over what the report returns. For example, the “Claim List” report provides a list of claims and their associated details, such as invoice number, payments, adjustments, and more. This report provides a wide range of criteria options so that you can return only claims that, for example, fall in a particular bill date range, or claims for a specific payer. The best part is that you can combine as many criteria parameters as you need to zoom in on just data that you want.
With these features, EZClaim makes reporting powerful and flexible, by giving you the power to instantly create real time reports that are as focused or broad as needed, and then exported in the exact format that you need them.
If you are ready to learn more about EZClaim reporting or have any questions about our leading medical billing software, schedule a consultation today or get in touch with our experts.

Jan 11, 2021 | Medical Billing Customer Service, Medical Billing Software Blog, Medical Billing Software Customer Service, MIPS Reporting, Revenue
It goes without saying that 2020 will go down in the history books as unprecedented for us at EZClaim. Still, we worked hard to stay positive and navigate the storm by offering resources to you, our clients, the content that matters to you. As an end-of-year bonus, and a ‘kick-off’ for 2021, we reviewed the blogs and social posts you read and reacted to the most and thought we would share them.
So, here are the best blog posts of 2020:
#1: How to Improve Medical Billing Revenues
As a medical billing company, we work hard to understand how we can help our clients increase their revenue and improve their billing process. Those who do this best are experts in the medical billing and coding industry. So, it makes complete sense that your interest peaked on our article concerning improving revenues. Enjoy reviewing our number one article of 2020! [ Click to read the post ].
#2: What Will Be New for E/M Coding in 2021?
Last year brought about a long list of changes to billing and coding, as well as, the medical industry as a whole. From the obvious boom in Telehealth, to the updates in evaluation and management services, those working in the industry were impacted immensely. Based on these shifts in industry and the impact on you, our clients, we thought a look into what was coming in 2021 would be useful—and so did you. You read, reacted, and shared the value of this content with others. Now we are sending you a reminder that this was our number two article for the year. [ Click to read the post ].
#3: Collecting Payments from Patients. Find Out How.
No matter how chaotic things get, there is still a practical side of our industry that needs to be addressed. That is why we worked to keep the focus on the basics, speaking about the ‘bread and butter’ of our industry, collections. In this practical article, we focused on the keys to educating the patient and how doing so will help keep you ahead of the collection as a whole. [ Click to read the post ].
#4: Reports – Nuisance or Necessity?
At the end of the day, you want to go home and no one wants to be stuck in the office doing double-duty on reports. You know as well as we, that getting reports done correctly the first time is key to reducing stress and going home happy. That is why we distilled some of the keys in running reports that would make your life more straightforward. The fourth article on our list will do just that by helping you make sure the dates, details, and destination of your reports are in the right place. [ Click to read the post ].
#5: Why Do I Have A Balance? – Patient Payments
Saving the best for last, especially as we approach tax season, we come in with our final of our best of 2020 by talking about balances. Every practice ends up spending those final hours of the year figuring out where those dollars and cents went. In this article, we gave you tips on deductibles, co-pays, and max out-of-pocket that helps your bottom line. Closing out 2020, don’t miss a few keys to help you balance the books. [ Click to read the post ].
These are EZClaim’s best blog posts of 2020, but these were not the only blog posts we did. So, if you would like to explore the other blog posts we did, click here for our blog page.
————————-
ABOUT EZCLAIM:
EZClaim is a medical billing and scheduling software company that provides a best-in-class product, with correspondingly exceptional service and support. Combined, they help improve medical billing revenues. To learn more, visit EZClaim’s website, e-mail support, or call a sales representative today at 877.650.0904.