Aug 11, 2020 | Features, Medical Billing Customer Service, Partner
Which is the BEST kind of Medical Billing Software? “All-in-One” or “Specialized”?
When considering WHICH medical billing solution they should use, practices wonder which is best, an “all-in-one” solution or specialized software. Well, the following are a few important pros and cons to consider when making a choice between these solutions.
ALL-IN-ONE:
An “all-in-one” system tries to provide a single, comprehensive solution that offers functionality for the major areas of the practice—Practice Management (PM), Electronic Medical/Health Records (EMR/EHR), and Revenue Cycle Management (RCM)—accessed from one central point. It has features like clinical notes, patient information, and history, diagnosis and treatments, scheduling, appointment reminders, reports, patient educational resources, as well as a medical billing section.
PROS:
• Most of what a practice need is included in the system
• There is no need to be concerned with multiple integrations or vendors
CONS:
• Tends to have a higher ‘entry’ cost
• Usually designed for the “middle-of-the-road,” therefore sometimes doesn’t properly address specific needs of a practice
• Sometimes, the practice is left paying for additional customizations to fit their particular needs
SPECIALIZED SOFTWARE:
Specialized medical billing software, on the other hand, is particularly programmed to maintain billing details of tests, procedures, examinations, diagnoses, and treatments conducted on patients. However, many specialized software providers extend their scope to include features like practice management, scheduling, and other administrative and clinical functions (that are generally a part of EHR software systems) by partnering with other specialty software companies—creating a “best-in-class” solution.
PROS:
• Integrating multiple “best-in-class” software packages—each taking a much more focused approach—creates an offering with much more in-depth capabilities
• Usually are more ‘nimble’ in responding to industry and regulatory changes
• More ’scalable’ in supporting the growth of a practice
CONS:
• Most of the time the practice has to deal with multiple vendors
CONCLUSION:
Where “all-in-one” solutions offer a wide breadth of capabilities across the business, they usually also lack focus, depth, and sophistication. “All-in-one” solutions are usually only efficient in one area, with the other areas tend to be ‘compromised’ and not fully developed. Then, when it comes to flexibility, they tend to be slow to adapt to changing practice needs.
Specialized software, however, typically offer a more efficient experience, with each ‘component’ streamlined and designed with a specific purpose in mind. Their focus on limiting the software scope makes them flexible and easy to use.
EZClaim—a leading software package in medical billing and practice management—has made it easier for the medical practice to have the benefit of a “all-inclusive” solution. They have created the best of both worlds by taking on the responsibility of integrating the “best-of-breed” into a harmonized “best-of-class” offering that allows the practice to pick and choose for their specific needs. The seamless integration of partner products and services ensures the practice does not have to give up robustness and flexibility for a simplified “all-in-one” solution, and it further enhances the practice’s workflow.
As a specific example, one of EZClaim’s partners is TriZetto Provider Solutions (TPS), a provider that seamlessly blends claims processing with revenue management and analytics software, so the practice can get paid faster, and more accurately.
Today, the practice can get the benefit of all the power and ease of use of EZClaim’s medical billing software and all the access and security that is needed when dealing with personal records by using TPS—which includes patient access, claims and denials management, patient financials, and advisory services.
The powerful integration between EZClaim and TPS efficiently adds functionality to the practice. Now the practice can gain deeper insight into the claim lifecycle, and take the proper steps to improve the overall health of the practice. The right ‘integrated’ solution makes all the difference!
So, if your practice needs more confident billing, after payments, and more informed decisions, but the power of EZClaim and TPS to work for your practice with the integrated suite of revenue cycle solutions.
In addition to TPS, EZClaim has tightly integrated a variety of of ‘components’ to be able to offer an “all-inclusive” best-in-class solution for a medical practice’s needs: Electronic Health Records (EHR), Clearinghouse, statement and payment services, HIPPA compliance, claims scrubbing, appointment reminders, and inventory management. It has partnered with a variety of providers like QuickEMR, BestNotes, and PracticeFusion [ Click here for an entire list of EZClaim’s partners ].
It is important to note that an “all-in-one” solution does not usually include the Clearinghouse portion that TPS offers. The powerful integration between EZClaim, TPS, and EZClaim’s EMR partners, efficiently adds functionality to ANY practice!
If you are considering the best course of action to meet your practice’s needs, consider using EZClaim by downloading a FREE TRIAL or contact one of their product specialists today to explore all the options for how to best solve your practice’s operational challenges, and grow your business.
For details and features about EZClaim’s medical billing software, visit their website.
Jul 14, 2020 | Health eFilings, MIPS Reporting, Partner, Revenue
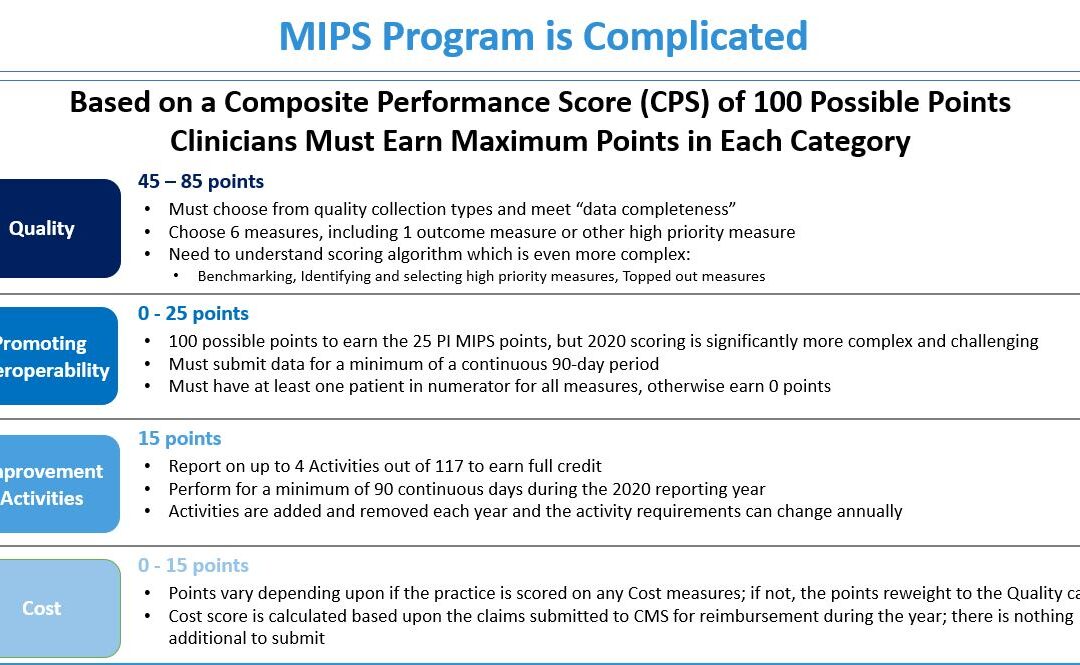
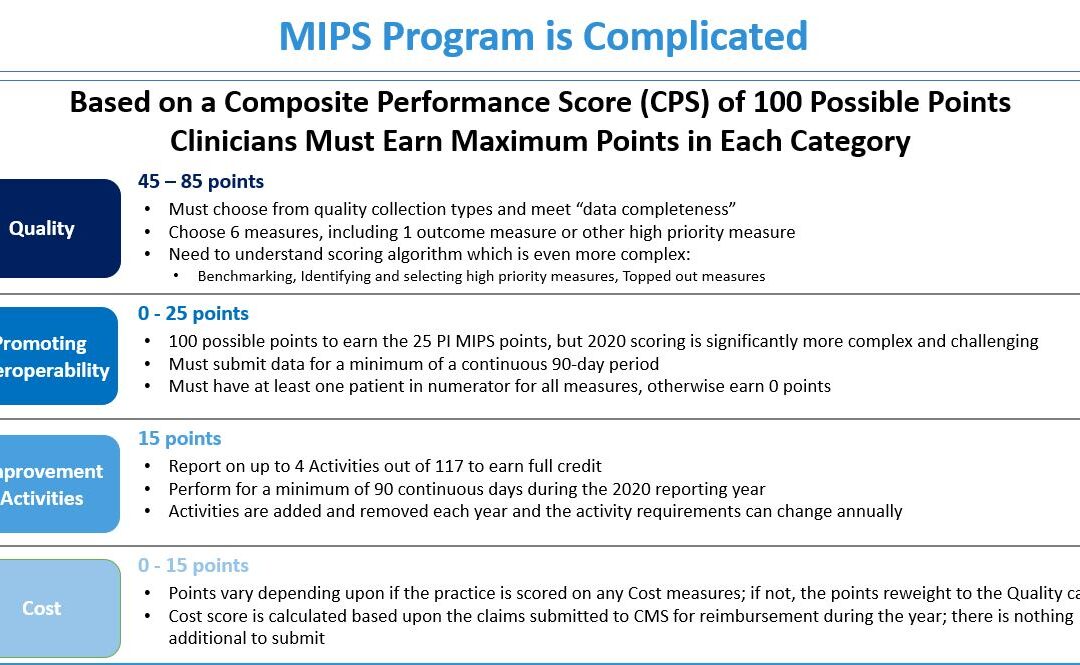
The 2020 MIPS reporting is already half done, and given that MIPS (Merit-based Incentive Payment System) is a points-based program, the goal is to earn as many points as possible to avoid this year’s 9% penalty and potentially even earn a positive payment adjustment. However, earning the 45 points necessary to avoid the penalty for the 2020 reporting period will be no easy feat. With over half of the reporting period already behind us, it is imperative you ACT NOW so you don’t find yourself in a position later in the year that you can’t recover from in terms of earning points.
With all the complexities and nuances of the program, it’s challenging to know what you can do to impact your score. Here are three critical actions to take right now so that you will still optimize your ability to earn points for the 2020 reporting period:
1. Focus on the Quality Category
There are various points available within each of the categories and the Quality Category has the most points associated with it. Based on a number of factors, the category is worth anywhere from 45 to 85 points. This is a critical category to be focused on throughout the year, so now is the time to ensure that you are tracking all relevant data so that it can be properly reported on within your submission.
2. Understand the Timeframe Requirements
Two of these categories, Promoting Interoperability and Improvement Activities, have timeframe requirements where you must perform for a minimum of 90 continuous days. These are not easy categories in which to be successful and so if you wait too long in the year you will find it impossible to put the right actions in place in order to complete the activities necessary to earn any of the points in these categories.
3. Choose the Right Reporting Methodology
Not all reporting methodologies are the same and the reporting methodology you select has a significant impact on the points you could earn. Additionally, there is strategic maneuvering that can be done throughout the reporting period with exemptions and reweighting of points that can set you up to optimize your performance and your score. Therefore, you must select a reporting partner that will help you earn the most points available and leverages technology to facilitate the ease, accuracy, and completeness of tracking and reporting to maximize your score. Reporting via a CEHRT, like Health eFilings, is the best approach because it optimizes the points that could be earned and therefore, maximizes Medicare reimbursements.
Health eFilings is a certified EHR technology (CEHRT) and the national leader in automated MIPS reporting. Their cloud-based ONC-certified software fully automates the reporting process. Because Health eFilings’ service is an end-to-end electronic solution that doesn’t require any IT resources, administrative support, or workflow changes from you, the practice will save significant time while maximizing its financial upside.
To learn more about how to properly perform your 2020 MIPS reporting, contact EZClaim’s partner, Health eFilings, so they can help before it’s too late!
For details and features about EZClaim’s medical billing software, or general information about the company, visit their website.
[ Written by Sarah Reiter, SVP Strategic Partnerships, Health eFilings ]

Jul 14, 2020 | Alpha II, MIPS Reporting, Partner, Webinar
Join this MIPS Reporting Webinar to be sure you are up to speed on the latest updates and changes.
Now that the MIPS (Merit-based Incentive Payment System) submission period is drawing to a close, join our partner, Alpha II, as they review the updates and changes for MIPS reporting in 2020. This session will discuss important program updates for 2020 reporting including:
• Eligibility requirements
• Performance thresholds
• Payment adjustments
• Performance category weighting
• Measure updates and more…
MIPS Reporting Webinar details:
Start reporting correctly now to ensure success for the 2020 performance year!

Jul 14, 2020 | Administrative Safeguards, Uncategorized
Credit card collections are a BIG part of any successful medical practice, and there has been a shift, in the last decade, that more insurance policies are adding co-pays with higher deductibles—which makes getting paid even more challenging.1 One industry report said that “73% of physicians shared that it typically takes at least one month to collect a payment, and 12% of their patients wait more than three months to pay.”2 With the current trend, more medical practices and their billing departments (or outsourced billing firms) are going the route of processing payment via credit cards, which has its PROS and CONS.
In light of this new information, the following are a few pros and cons for credit card processing that we anticipate in the near future and some insights for choosing the best billing software that supports the credit card processing needs of medical practices:
- PRO: To protect against the dangers of stolen data, fraud, or other compromises in security, practices should seek out medical billing software that has credit card processing built-in, which can help safeguard against these dangers.
- CON: Security is a big risk, and a leak in data leading to stolen funds can end up in a physician paying out-of-pocket for the breach. It is also important to note that breach of credit card data is also considered a violation under the federal Health Insurance Portability and Accountability Act (HIPAA).
- PRO: Implementing credit card processing will reduce long waiting periods for payments from the majority of your patients, and will also reduce the additional effort your billing staff has to extend to collect on overdue notices.
- CON: Practices cannot require patients to share their credit card information to receive medical care, and even if patients do share their credit card information, physicians cannot continue to charge the credit card without a patient’s consent.
- PRO: Physicians can end the process of being a “line of credit” to unpaid or underpaid claims, and collect on funds immediately.
- CON: You will need to implement internal processes that include, but are not limited to proper personal information storage and security, establishing guidelines on maximum percentages charged per bill, and personal consent forms.
Overall, there are definitely MORE ‘PROS’ than cons for implementing credit card processing for your medical practice, and all the trends are pointing to this being the PREFERRED METHOD of payment in the near future. EZClaim is proud to announce that it will release an integrated credit card processing solution, EZClaimPay, that is backed by a national merchant services vendor. [ EZClaim will be sharing more details about EZClaimPay in the weeks to come, via their social media platforms, their monthly newsletter, direct communications, and more ].
In addition to the credit card collections PROS and CONS above, we reached out to one of our partners, Live Compliance, to gather some regulatory and security advice. They suggested the following:
- When accessing, transmitting, storing, or receiving any Protected Health Information (PHI), the Health and Human Services (HHS) Office of Civil Rights (OCR) mandates that you are to maintain HIPAA compliance.
- When accepting, processing, or maintaining credit card information and debit card information, you must ensure that your organization is PCI DSS compliant (Payment Card Industry Data Security Standard).
- In addition to the above Federal regulatory requirements, most states require privacy and security compliance requirements to be implemented, along with strict adherence to the privacy of Personally Identifiable Information (PII) and Breach Notification requirements.
For more information on your compliance requirements, visit Live Compliance for a Free Organization Assessment to identify and uncover your organization’s vulnerabilities.
If you are not a current customer of EZClaim, we would very much like to connect with you. You can either schedule a one-on-one consultation with our sales team, view a recorded demo, or download a FREE 30-day trial right now. For detailed product features or general information about EZClaim, visit our website at ezclaim.com.
[ NOTE: If you would like a quote on the upcoming merchant services, please e-mail sales@ezclaim.com your last three merchant statements. For more on our ongoing updates and industry news, you can follow EZClaim on Facebook and LinkedIn ].
Source Material:
1 – America’s Health Insurance Plans” report that there were 20.2 million co-pays in 2017, which was up tremendously from just over 1 million in 2005.
2 – Source: From InstaMed’s annual “Trends in Healthcare Payments” report.
> For more on this topic, read a previous article, “Why Do I Have A Balance? – Patient Payments”
Jun 10, 2020 | Partner, Support and Training
Home care employers are confronting difficult questions regarding how to handle labor and management relations, leave and accommodation, safety and health, and other employment issues.
Littler, a law firm that focuses on labor and employment law, has produced an extensive home care industry FAQ document (41 pages) called “Home Care Industry Coronavirus (COVID-19) Employer Frequently Asked Questions.“ It provides general advice to help address some of the more common questions that home care employers currently face due to the COVID-19 pandemic.
CONTENTS:
• Client/Patient Privacy/HIPAA
• FFCRA
• CARES Act (Including PPP)
• Unemployment
• ADA Considerations
• Leaves of Absence
• Wage & Hour
• WARN Act
• Workers’ Compensation
• Health and Safety
• Labor/Management Relations
• Employee Relations
Litter also has a specific page on their website that provides a useful resource for employers to learn how COVID-19 is affecting various aspects of employment law, and how different jurisdictions are addressing the outbreak. Because the COVID-19 situation is dynamic, with new governmental measures each day, Litter suggests that employers consult with counsel for the latest developments and updated guidance on this topic. Click here to view their resource page.
This information was sent to us by one of EZClaim’s premier partners, AxisCare, who provides a home care system designed with the workflow of a private duty agency in mind. AxisCare provides a scheduling software solution that features a GPS mobile app, automatic invoicing, billing and payroll integrations, custom forms, custom reporting, and more. For more details about their all-in-one home care software solution, view their website.
Since developments related to the COVID-19 pandemic are evolving on a daily basis, EZClaim is continuing to discover resources that will assist its clients in understanding these developments. As always, we are here to support your medical billing needs and hope you are safe and well in this challenging time.
For general information about EZClaim, or details about the features of our medical billing software, visit our website.
Click here to download the PDF